- Visibility 166 Views
- Downloads 22 Downloads
- DOI 10.18231/j.jco.2022.005
-
CrossMark
- Citation
Treatment of maxillary lateral incisor-canine pseudotransposition: A case report
- Author Details:
-
T. P. Chaturevdi
-
Vipul Kumar Sharma *
-
Alka Singh
Introduction
The term transposition is used to refer to an interchange in the position of 2 adjacent teeth within the same quadrant of the dental arch.[1] Transposition may be complete or incomplete.[2] Incomplete transposition, both the crowns and the entire root structures of the involved teeth are found parallel in their transposed positions. In incomplete transposition (also called “pseudo” or “partial” transposition) the crowns may be transposed while the root apices remain in their normal positions. Alternatively, the crowns may be in the correct order while the root apices are transposed. In addition, the crowns and roots of the 2 involved teeth may completely superimpose each other on normally projected radiographs. Prevalence of transposition varies (<1%) with 0.43% in Indian population.[3], [4], [5] Transposition affects the maxillary dentition (68.5%-76%) more frequently than the mandibular dentition. Maxillary canine-lateral incisor transposition is the second most common type of transposition (20%-42%) after maxillary canine-first premolar transposition (55-70%). Unilateral transposition has been reported more often than bilateral transposition, with the left side being somewhat more frequently involved than the right side.[6] Transpositions have been found more often in females than in males and in the maxilla than in the mandible.[3] Dentofacial trauma in the deciduous dentition, with subsequent drifting of the developing permanent teeth is the most common etiologic factor of maxillary canine-lateral incisor transposition.[4] The only dental anomaly that has an apparent association with maxillary canine-lateral incisor transposition is increased third molar agenesis.[3] Treatment of maxillary canine-lateral incisor transposition depends on many factors like the condition of root of central incisors, shape of lateral incisors, need of extraction because of either severe crowding or profile improvement etc. Here, we are going to present management of a rare case report of maxillary right lateral incisor-canine pseudotransposition with minimum available space and agenesis of mandibular third molars.
Case Report
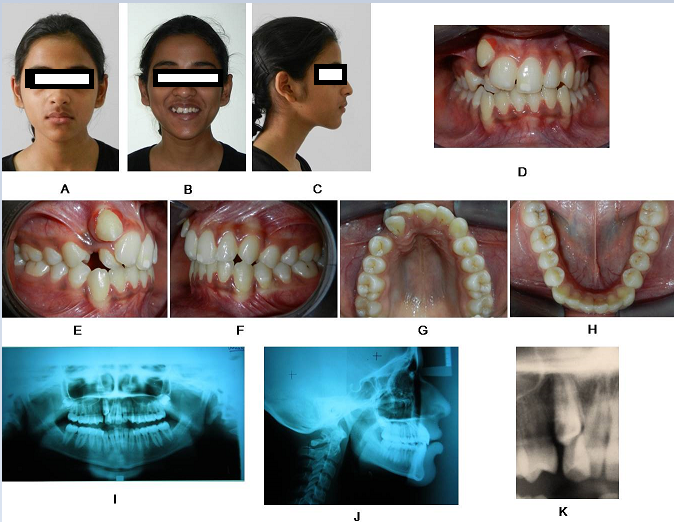
15 years old female came to the Department of Orthodontics and Dentofacial Orthopaedics, FODS, KGMU, Lucknow with the chief complaint of irregularity in upper front teeth. Her medical and dental history was not significant. Extraoral examination showed well-proportioned face, pleasing facial profile with competent lips and harmonious nasolabial angle. Intraoral examination showed Class I molar relation, 1 mm of overjet, 2 mm of overbite, labial displaced maxillary right canine overlapped with lateral incisor and 3 mm of maxillary midline deviation on right side. Both the mandibular third molars were absent. Radiographic examination (orthopantomogram and intraoral periapical radiograph) revealed pseudotransposition of maxillary right canine and lateral incisor. ([Figure 1]) Available space to align maxillary right canine was 3 mm. Cephalometric findings suggest that skeletal, dental and soft tissue readings were within normal limits. ([Table 1]) Carey’s analysis showed -5 mm discrepancy in the maxillary arch. Ashley Howe’s analysis showed adequate premolar basal arch width for expansion of maxillary arch. (Premolar basal arch width percentage=42%)
Treatment Objectives
Treatment objectives were correction of maxillary right canine-lateral incisor pseudotransposition, correction of maxillary dental midline deviation within soft tissue envelope.
Treatment plan and treatment progress
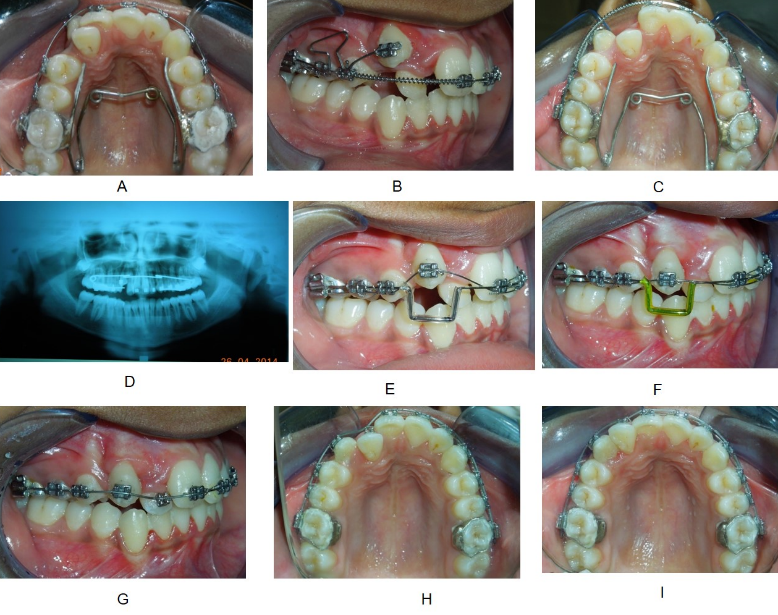
Based on analysis of diagnostic records, non-extraction treatment plan was selected. Arch expansion was planned in the maxillary arch to create space for maxillary right canine. Standard edgewise appliance (022”x028” slot) was bonded in maxillary arch and quad helix (038 blue elgiloy) installed simultaneously. ([Figure 2] A-B) Alignment and leveling was started with 0.016” thermal NiTi followed by 0.017”x0.025” thermal NiTi and 0.019”x0.025” stainless steel for 5 months.
|
Measurements |
Normal |
Pre-treatment |
Post-treatment |
|
Horizontal skeletal |
|
|
|
|
SNA (0) |
82 |
81 |
79 |
|
SNB (0) |
80 |
80 |
77 |
|
ANB (0) |
2 |
1 |
2 |
|
Facial angle (0) |
87 |
86 |
84 |
|
Wits appraisal (mm) |
0-1 |
-6 |
2 |
|
Vertical skeletal |
|
|
|
|
FMA (0) |
25 |
28 |
30 |
|
Go-Gn to SN (0) |
32 |
34 |
35 |
|
Occlusal plane to SN (0) |
14 |
16 |
12 |
|
Maxillary incisors |
|
|
|
|
Mx.1 to A-Pog (mm) |
2.7 |
7 |
9 |
|
Mx.1 to NA (0/mm) |
4 / 22 |
6/23 |
6/28 |
|
Mx 1 to SN (0) |
104 ± 7 |
101 |
107 |
|
Mandibular incisors |
|
|
|
|
Md.1 to A Pog.(mm) |
1+2 |
3 |
4 |
|
Md.1 to NB (0/mm) |
4 / 25 |
4/20 |
4/23 |
|
IMPA (0) |
90 |
88 |
90 |
|
Interincisal angle (0) |
135 |
137 |
128 |
|
Soft tissue |
|
|
|
|
Rickett’s E-line(upper) (mm) |
-4 |
-3 |
-2 |
|
Rickett’s E-line(lower) (mm) |
-2 |
1 |
-2 |
|
H Angle (0) |
10 (7-15) |
16 |
16 |
|
Soft tissue subnasion N to H-Line (mm) |
5 (3-7) |
6 |
5 |
|
Lower lip to H-line (mm) |
1-2 |
3 |
1 |
|
Naso-labial Angle (0) |
94 -110 |
107 |
98 |
|
Upper lip length (mm) |
24 |
21 |
23 |
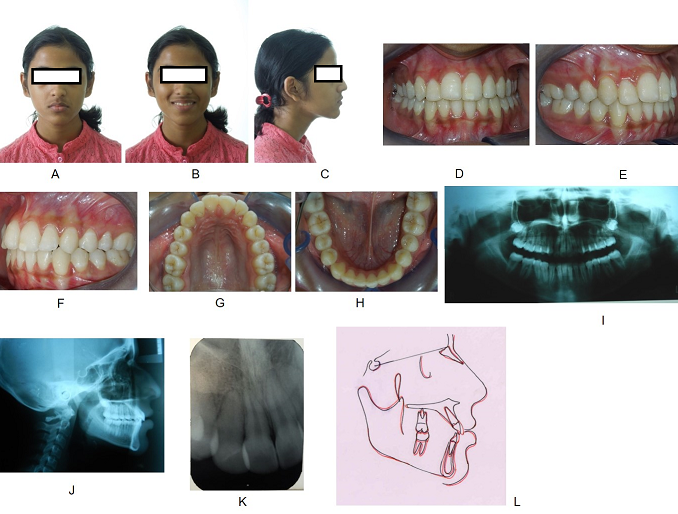
Quad helix was reactivated during alignment and leveling. Open coil spring (0.010”x0.030” NiTi) was compressed between maxillary right central incisor and first premolar to create space for canine and correct deviated midline simultaneously for 3 months. T-loop was ligated to retract the transposed canine. ([Figure 2] C-G) After retraction of canine, open coil spring, T-loop and quad helix were removed. Mid-treatment orthopantomogram was taken to see root parallelism. ([Figure 2] H) was done from right central incisor to left first molar and right first premolar to right first molar with ligature wire. Stabilising wire (0.019”x0.025” stainless steel) with mesial and distal step to the transposed canine and 016 thermal NiTi overlay wire were ligated. ([Figure 3] A-E) After aligning the canine into the arch, maxillary right lateral incisor was bonded and 0.016”x0.022” CuNiTi ligated followed by 0.019”x0.025” NiTi and 0.019”x0.025” stainless steel. ([Figure 3] F-I) Labial root torquing of lateral incisor was done. Final finishing and detailing was done after bonding mandibular arch.
After 15 months of treatment, case was debonded and removable circumferential retainer was given in upper arch. Good esthetic smile was achieved. Minimum soft tissue changes were seen after completion of treatment. ([Table 1] )There was no significant root resorption of upper right lateral incisor.
Discussion
This patient presented with a challenging case of pseudotransposition of the right maxillary lateral incisor and canine with minimum space availability for correction. This is a typical case of mandibular third molar agenesis associated with transposition and right side involvement. There are three different treatment options for transposition i.e., extraction, maintenance, and correction.[7] Complete transpositions require complex and often protracted treatment plans with no guarantee of success. Correction of transposed canines may be limited by mechanical considerations, alveolar bone support, gingival health, treatment duration, age of the patient, financial and other considerations. Possibility of correcting tooth transposition is greater in maxilla than mandible because of adequate amount of bone. Maintaining tooth order is recommended in maxillary canine/first premolar transposition because of tooth resemblance but may result in aesthetic compromise. [8] The necessity of moving the lateral incisor palatally has been discussed before in case of maxillary lateral incisor-canine transposition.[4] The treatment would be finished with buccal movement of the palatally displaced teeth. Doing so, avoid potential root interferences and prevent potential loss of the cortical plate by allowing the canine to come into the arch rather than too far labially.[9] In this case, we had two favorable conditions to correct it with the non-extraction method; (1) adequate premolar basal arch width to expand the maxillary arch (2) maxillary right lateral incisor is already palatally placed. Transposition should be managed as a part of the comprehensive treatment plan. Only segmented appliances allow the application of well-defined and frictionless biomechanical force systems for highly controlled tooth movement; cantilevers and various types of loops can be designed according to the laws of equilibrium. The results are highly predictable, and undesirable side effects (round-tripping, iatrogenic damage) can be minimized and easily monitored.[10] The low load-deflection rate and wide range of activation of nickel-titanium springs and beta-titanium alloy wires enable them to maintain high constancy of both force and moments during orthodontic therapy without the need for frequent reactivations and appliance adjustments.
Conclusion
When the teeth involved in the transposition are fully erupted and completely or almost completely aligned in the transposed position, a satisfactory result can be obtained by maintaining the transposition, and correction, even if possible, would not always be advisable from a cost-benefit point of view. Care should be taken for root resorption of lateral incisor during correction of transposition. Early recognition (6-8 years) and interceptive measures such deciduous teeth extraction and tooth guidance could facilitate further treatment.
Source of Funding
None.
Conflict of Interest
None.
References
- Y Shapira, M M Kuftinec. Tooth transpositions-a review of the literature and treatment considerations. Angle Orthod 1989. [Google Scholar] [Crossref]
- Y Shapira, M M Kuftinec. Maxillary canine-lateral incisor transposition-Orthodontic management. Am J Orthod Dentofac Orthop 1989. [Google Scholar] [Crossref]
- A Chattopadhyay, K Srinivas. Transposition of teeth and genetic etiology. Angle Orthod 1996. [Google Scholar] [Crossref]
- F Maia. Orthodontic correction of a transposed maxillary canine and lateral incisor. Angle Orthod 2000. [Google Scholar] [Crossref]
- H Yilmaz, H Turkkahraman, M Sain. Prevalence of tooth transpositions and associated dental anomalies in a Turkish population. Dentomaxillofac Radiol 2005. [Google Scholar] [Crossref]
- N Ely, M Sherrif, M Cobourne. Dental transposition as a disorder of genetic origin. Eur J Orthod 2006. [Google Scholar] [Crossref]
- S Peck, L Peck. Classification of maxillary tooth transpositions. Am J Orthod Dentofac Orthop 1995. [Google Scholar] [Crossref]
- M R Joshi, N A Bhatt. Canine transposition. Oral Surg Oral Med. Oral Pathol 1971. [Google Scholar] [Crossref]
- Y Shapira. Transposition of canines. J Am Dent Assoc 1980. [Google Scholar]
- S Peck, L Peck, M Kataja. Concomitant occurrence of canine malpositions and tooth agenesis: evidence of orofacial genetic fields. Am J Orthod Dentofac Orthop 2002. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Chaturevdi TP, Sharma VK, Singh A. Treatment of maxillary lateral incisor-canine pseudotransposition: A case report [Internet]. J Contemp Orthod. 2022 [cited 2025 Sep 11];6(1):25-28. Available from: https://doi.org/10.18231/j.jco.2022.005
APA
Chaturevdi, T. P., Sharma, V. K., Singh, A. (2022). Treatment of maxillary lateral incisor-canine pseudotransposition: A case report. J Contemp Orthod, 6(1), 25-28. https://doi.org/10.18231/j.jco.2022.005
MLA
Chaturevdi, T. P., Sharma, Vipul Kumar, Singh, Alka. "Treatment of maxillary lateral incisor-canine pseudotransposition: A case report." J Contemp Orthod, vol. 6, no. 1, 2022, pp. 25-28. https://doi.org/10.18231/j.jco.2022.005
Chicago
Chaturevdi, T. P., Sharma, V. K., Singh, A.. "Treatment of maxillary lateral incisor-canine pseudotransposition: A case report." J Contemp Orthod 6, no. 1 (2022): 25-28. https://doi.org/10.18231/j.jco.2022.005
