Introduction
Patients in young age group now-a-days are very concerned about orthodontic treatment and the time needed to correct, being their prime priority.1 Four primary factors of open bite are Thumb or pacifier sucking, Tongue thrusting, Temporomandibular joint disorder, Skeletal problem. In orthodontics, one of the challenging and difficult cases to treat is anterior open-bite. Some main morphological characteristics of this type of malocclusion are; increased lower facial height and steep mandibular plane which mostly leads to over-erupted maxillary posterior dentition.2, 3, 4, 5 Conventional fixed orthodontic treatment requires 2-3 years to get completed which indirectly leads to high risk of caries, root resorption, and reduced patient compliance,6, 7, 8, 9, 10, 11, 12 To reduce the treatment time different methods such as low-level laser therapy, orthodontic camouflage with premolars or first molars extraction, pulsed electromagnetic fields, electrical currents, micro-osteoperforation, corticotomy, distraction osteogenesis, and mechanical vibration can be used combined with conventional orthodontics.13, 14, 15, 16, 17, 18, 19, 20, 21, 22 Studies have shown that open bite treated with extraction has greater stability of the overbite than open-bite non-extraction treatment.23 In orthodontics, micro-osteoperforation (MOP) can be done to perforate the bone around the teeth with small-pinhole perforation to accelerate the rate of tooth movement during orthodontic treatment. This procedure activates the release of cytokines that in turn recruit osteoclasts to the area to increase the rate of bone resorption.24 Tongue thrusting is one of the commonest causes of anterior open bite. Anterior tongue posture or macroglossia are the two main reasons of tongue thrusting habit. Habit breaking appliances such as tongue crib or lingual tongue restraining spikes can be given in growing age to correct anterior tongue thrusting. This gives a negative reinforcement to the tongue and which results in new corrected tongue posture. Once the growth ceases, the new corrected tongue posture is very difficult to develop and hence posttreatment retention is one of the major concerns for an orthodontist.25 The goal of this case report is to correct anterior open-bite due to tongue thrusting with rapid and effective method of extraction and micro-osteoperforation facilitated orthodontic treatment of a young patient.
Case Report
A 13-year-old female patient reported with the chief complaint of inability to close the mouth and forwardly placed teeth in front region of the jaw. She had no relevant medical history, good oral hygiene and periodontal health, with a restoration done 1-year-ago.
Etiology
The patient had a habit of mouth breathing with anterior tongue thrust. The habit of tongue thrust was due to enlarged tongue size (macroglossia) with no abnormality in speech.
Extraoral examination
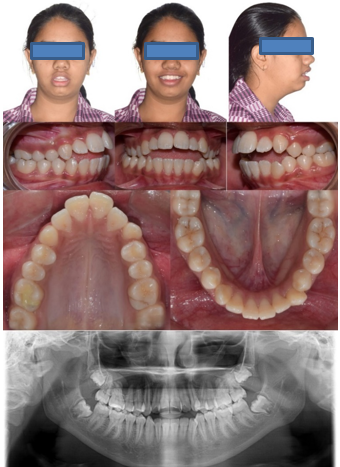
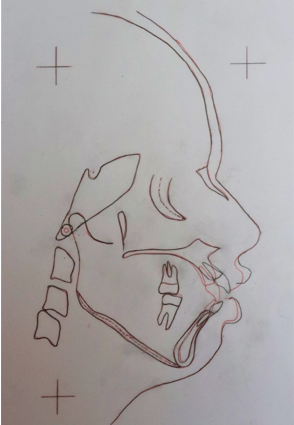
No gross facial asymmetry with mesoprosopic face form. On profile examination, patient had convex facial profile with symmetric and flat smile and incompetent lips with 100% maxillary incisor display while smiling (Figure 1).
Intraoral examination
All teeth in the upper and lower arch were present except for the third molars. Ovoid shaped, upper and lower arches. Mucogingival frenal attachment, satisfactory gingival health and low caries risk. proclined upper and lower anterior teeth. Angle’s Class I malocclusion with anterior open bite and posterior crossbite due to narrow maxilla and canine relation is Class I on right side and not recordable on left side (Figure 1).
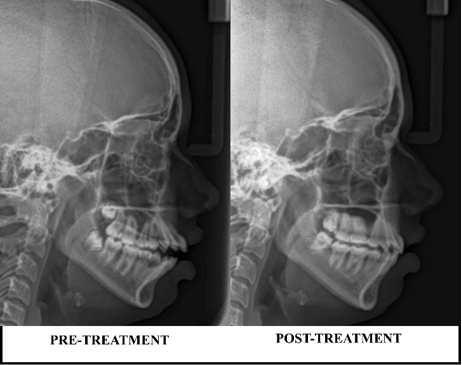
Functional examination
The patient showed oronasal breathing which was confirmed and tested by water holding test, and due to macroglossia a typical swallowing pattern was observed. Path of mandibular closure was normal with maximum mouth opening was 47mm. Increased overjet of 4mm and 8mm of anterior open bite. According to cephalometric analysis, patient had Class I skeletal bases, average growth pattern. The soft tissue analysis revealed both upper and lower lip protrusion. Nasolabial angle was acute and deep mentolabial angle (Figure 1, Figure 4; Table 1).
Treatment objectives
To eliminate the tongue-thrusting habit, improve facial profile and dental aesthetics, close anterior open-bite, correct proclination of upper and lower arch, establish interdigitation of both arch, achieve competence of lips with normal overjet and overbite.
Table 1
Cephalometric changes
Treatment plan
The treatment plan advised included comprehensive orthodontic treatment with fixed mechanotherapy to level and align maxillary and mandibular arch by eliminating crowding in both arch, correcting posterior crossbite along with closure of anterior open-bite. Extraction of all four first premolar to attain stability and to accelerate the tooth movement, micro-osteoperforation was carried out. To avoid mesialization of all first molars, second molars were also banded and compound anchorage was achieved.
Treatment progress
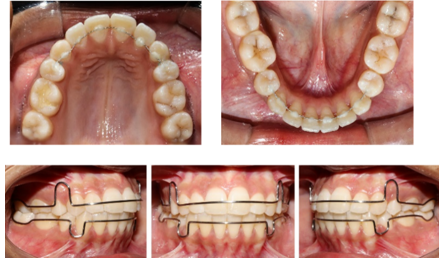
Begg’s bracket were bonded on lingual surface of 31, 32, 41, 42, 43 and lingual button on 11,21 respectively for correction of tongue thrusting habit. Quad helix was given to correct posterior crossbite with raised posterior bite with Glass Ionomer Cement (Figure 2.a, b), then 0.022” x 0.025” slot dimension preadjusted edgewise orthodontic fixed appliance of MBT prescription metal brackets were bonded in both the arches. Following wires were used during treatment sequentially 0.014”, 0.016”, 0.018”, 0.017” x 0.025” NiTi, 0.019” x 0.025” SS wire. After 4 months of full slot expression of wire and initial levelling and alignment, all first premolars were extracted, and after extraction, within 1 week retraction started and 2mm space were covered up during this 2 months of post extraction. Retraction speed decreased after healing of socket therefore planned for micro-osteoperforation was carried out on the distal aspect of all four canines to fastened up the retraction process (Figure 3).
Surgical procedure
Under local anaesthesia, 14, 44 were extracted and after 2 weeks 24, 34 were extracted. Immediately after extraction, canine to canine were consolidated and 0.019” x 0.025” SS arch wire was placed in both the arches. Within 1 week, crimpable hooks were placed between lateral incisor and canine in all the four quadrants; and a long elastomeric chain was placed from crimpable hook to molar hook for 2 months with replacement in every 20 days (Figure 3).
With the help of radiographs which were taken prior to micro-osteoperforation, along with the assessment of length and thickness of the attached gingiva, health of periodontium, closeness of the frenum, accessibility of the area of interest; micro-osteoperforation procedure was carried out to the distal aspect of all four canines under topical application of anaesthesia and local anaesthesia.
Approximately 5-6 mm penetration into the alveolar bone was done. The patient was prescribed antibiotic for 5 days after the procedure and advised to gargle with Betadine mouthwash for 1 week to prevent infection and inflammation. Immediately after micro-osteoperforation procedure, canine-to-canine consolidated 0.019” x 0.025” SS arch wire were placed in both the arches, and for next 7 months for retraction with active tie back and replaced every 20 days subsequently to utilize regional accelerated phenomena [RAP] (Figure 3).
Finishing procedure
The total active treatment period was only 9 months. With the help of N-shaped elastics posteriorly and anterior box elastic were given for the next 2 months and proper interdigitation was achieved. Fixed appliances were removed and fixed retainers were placed in both the arches (Figure 3).
Treatment outcome
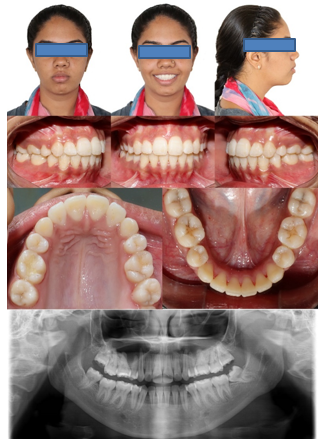
At the end of treatment, facial profile, dental aesthetics, vertical and sagittal relationship were improved and the anterior open-bite was corrected (Figure 4, Figure 5). Angle’s Class I molar and canine relation with normal overbite and overjet were achieved (Figure 5, Figure 8).
Posterior crossbite was corrected. Pleasing smile in the posttreatment extraoral and intraoral photographs. Posttreatment lateral cephalometric analysis and superimpositions showed the difference between pre-and-post treatment changes in both skeletal and dental discrepancies (Figure 1, Figure 4, Figure 5, Figure 8 and Table 1). In the posttreatment panoramic radiograph, slight apical root resorption was seen in maxillary anterior and erupted maxillary and mandibular third molars as well.
Retention
Glossectomy was advised to the patient to correct the etiology of macroglossia of the anterior open-bite after treatment but the patient was not willing for any further surgical intervention. Fixed lingual retainer were bonded from second premolar to second premolar in both arches along with removable Begg’s wrap around retainer to reduce the chances of relapse (Figure 6).
Follow up after one-year, showed stable post-retention results (Figure 7).
Discussion
Dento-alveolar anterior open bite is mostly characterised by macroglossia which leads to anterior tongue thrusting habit.25 Henceforth, a habit breaking appliance is given, as in our case we had given Begg’s brackets in lower anteriors and lingual buttons in upper central incisors. It is known that the orthodontic therapy with all four first premolar extraction along with micro-osteoperforation reduces the period of conventional orthodontic treatment. As studies reported in literature, the stability of anterior open-bite in extraction cases is more as compared to non-extraction cases and the rate of tooth movement is rapid in cases of micro-osteoperforation.23, 24 The total treatment time was only almost half as compared to routine orthodontic therapies.26 Bone mineral density is related to the rate of orthodontic tooth movement. Tooth movement in young patients is faster than in adults.27
The micro-osteoperforation is minimally invasive flapless surgical interventions which increased bone remodelling, osteoclastic activity and induced faster orthodontic tooth movement.28 According to many researchers, there was no significant differences in terms of pain severity levels after micro-osteoperforation.29 As advocated by Wilcko et al. the conventional orthodontic forces explained the rapid tooth movement due to Regional Acceleratory Phenomenon.30, 31
Conclusion
Extraction of all four first premolars along with Micro-osteoperforation assisted orthodontics is an effective method in patients with severe malocclusion whose priority is reduced treatment time.
It is important to carefully monitor teeth and surrounding periodontium to avoid risk of devitalization of the teeth and periodontal damage.
Declaration of patient consent
It is certified by the authors, that all the appropriate patient consent forms have been obtained. The patient has given her consent about her photos and other clinical information to be reported in the journal. The patients have been assured that their names and initials will not be published and all the essential efforts will be made to conceal their identity, but anonymity cannot be guaranteed.