Introduction
All across the world, there are more and more adult patients receiving orthodontic care. Orthodontic therapy is no longer just a child's domain. According to the Journal of Clinical Orthodontics survey from 2013, they make up an average of 23% of orthodontic patients, up from 10% 15 years earlier.1 According to the definition of an adult, who is completely grown, most males who are 18 or older and most females who are 16 can be regarded as adults.2
Adult patients seek orthodontic treatment for a variety of reasons, including cosmetic concerns, psychological concerns, interdisciplinary treatment (periodontics, prosthetics), functional issues, or dysfunction of the temporomandibular joint. According to Musich, 25 percent of the 1370 adult orthodontic patients require comprehensive care, 70 percent require multidisciplinary care, and 5 percent don't require any orthodontic care at all.3
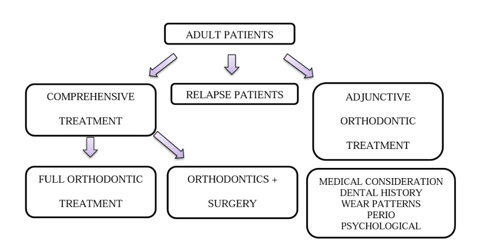
Adult patients can be divided into two groups: younger adults, who are typically under 35 and frequently in their 20s, and older adults, who are typically in their 40s and 50s.4 The first group looks for the most thorough orthodontic care and improvement. The second group, in contrast, pursues orthodontic treatment as an add-on technique to the significant periodontal & restorative objectives. However, the third group - the "relapse patients" - should now be taken into account. The alignment of many children and adolescents who got orthodontic treatment in the 1970s, 1980s, and 1990s—particularly the lower anterior teeth5—had relapsed, and they were looked for a second, frequently easier, orthodontic procedure to restore the alignment of the anterior teeth. (Figure 1)
Adjunctive orthodontic treatment for adults is, by definition, tooth movement carried out to facilitate other dental procedures necessary to control disease, restore function and/or enhance appearance.4, 5, 6 Treatment for excessive tooth wear, pulpit is associated with occlusal trauma, drifting of teeth after extraction, lack of tooth structure, cross bite or misalignment of anterior teeth, repositioning of adjacent teeth prior to implant restoration, and extruding tooth are all examples of adjunctive orthodontic procedures. The general dentist may be qualified to perform adjunctive treatment. As a result, the general dentist must be able to recognize the need for adjunctive treatment and provide it when needed.
Considerations for Adults Regarding Adjunctive Orthodontic Treatment
Adults frequently use a variety of drugs, some of which may affect tooth movement. Chronic usage of nonsteroidal anti-inflammatory medicines has been shown to impede or even prevent orthodontic tooth movement.7 Additionally, medications that affect bone turnover, such as bisphosphonates, which are commonly used to treat osteoporosis, might also impede tooth movement.8
It is generally known that orthodontic therapy can hasten periodontal disintegration when there is active periodontal disease present.9 According to data from the most recent national health survey conducted in the United States, 47 percent of persons over the age of 30 had periodontal disease that is actively progressing.10 Therefore, a complete periodontal examination should be performed on every adult patient before beginning orthodontic treatment, and active periodontal disease must managed before adjunctive orthodontic treatment.11, 12
Patients with uncontrolled diabetes who develop periodontal disease risk substantial bone loss. Patients should be made aware of the potential for gingival inflammation throughout therapy, and the course of action should be carefully planned with a periodontist.13 The length of orthodontic treatment has been greatly shortened thanks to the adoption of modern procedures like PAOO (Periodontally accelerated osteogenic orthodontics) and MAPA-cision,14 which have also improved treatment results.15 Because the apical movement of the tooth's Center of Resistance,16 enhances the moments produced by any pressures applied to the crowns of the teeth, situations where there has been bone loss necessitate careful adjustment of the orthodontic forces.
Adjunctive Versus Comprehensive Orthodontic Treatment
Table 1
Types of adult orthodontic treatment 17
Treatment Goals for Adjunctive Orthodontics
Improve the alveolar ridge contour next to the teeth and remove plaque-harboring areas to improve periodontal health.18
Create favourable crown-to-root ratios and place the teeth such that the long axes of the teeth so the path that occlusal forces follow.
-
Make restorative procedures easier by arranging the teeth so that:
Congenitally lacking teeth or hypodontia are conditions that jeopardize the patients' needs in terms of phonetics, aesthetics, and functionality. Results from additional orthodontic treatment techniques like orthodontic space regaining are predictable.19, 20 The primary complaint, medical assessment, psychological factors, and lifestyle should all be evaluated while evaluating an adult patient. The following goals involve gradually concentrating on the teeth, malocclusion, oral cavity, periodontium, and face.21
Orthodontic care for temporomandibular dysfunction (TMD) shouldn't be viewed as an additional kind of care.4
Even though tooth intrusion can be a significant component of comprehensive therapy for adults, due to the technical challenges and potential periodontal issues, it should definitely be handled only by an orthodontist. Lower incisor teeth that were overly extruded were best treated by reducing crown height, which has the added benefit of increasing the final crown-to-root ratio of the teeth. This is a general recommendation for treating adults with periodontal involvement and bone loss. When considering crown height reduction for other teeth, tooth-lip relationships must be taken into account.4
The anterior teeth's contact surfaces shouldn't be stripped of enamel in an attempt to achieve crowding of more than 3 to 4 mm. To provide room for the incisors' alignment, it may be useful to strip posterior teeth, although doing so necessitates the use of a full orthodontic appliance and is not a kind of adjunctive care.4
Planning for Diagnosis and Treatment
There are two processes involved in planning for adjunctive therapy:
Individual intraoral radiographs should typically be included in the records for the adult and dentally challenged population in addition to the panoramic film, which frequently suffices for younger and healthier patients. The panoramic radiograph does not provide enough information when there is active oral disease present.
Pre-treatment cephalometric radiographs are typically not needed for adjunctive orthodontics, but it is crucial to predict the effects of different tooth motions on facial aesthetics hence it is advised to take them when necessary. Planning adjunctive treatment can occasionally benefit greatly from the computer prediction techniques employed in comprehensive treatment. Due to the ease with which they allow for the planning of concomitant restorative operations, articulator-mounted casts are likely to be required.
Adjunctive Treatment With Biomechanical Thought
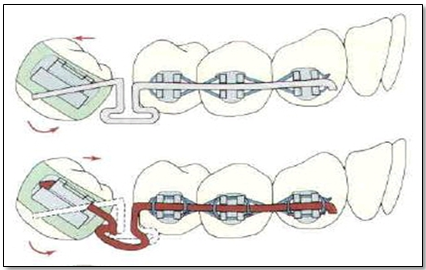
If the patient has lost some periodontal support, it is particularly especially essential to use light forces during space closure. For space closure in periodontally impaired adult patients, the segmented arch method with TMA T-loops were advised.22 In order to produce precisely regulated force against the teeth whose movement is required, the essential concept behind segmented arch therapy is to construct a stable anchor unit out of a number of teeth that were permanently attached to one another.
When using a partial fixed appliance for adjunctive therapy, the brackets are only placed in the ideal location on the teeth that need to be moved; the anchor system's remaining teeth are bracketed such that the arch wire slots are tightly spaced apart. The 22-slot edgewise appliance with twin brackets is preferred when a partial fixed appliance is to be utilized for adjunctive therapy, with the possible exception of aligning anterior teeth. The comparatively widse bracket helps control unwanted rotations and tipping, the rectangular bracket slot allows management of buccolingual axial inclinations, and the bigger slot size allows the use of stabilizing wires that are a little stiffer than typically could be utilized in comprehensive treatment.
Recent advancements in clear aligner therapy have produced a successfudl removable appliance that may be well suited for anterior tooth alignment. For adjunctive (or comprehensive) treatment, standard plastic-and-wire removable equipment are rarely sufficient. They frequently cause discomfort and are probably worn for too few hours each day to be useful. With clear aligners, patient compliance increases while discomfort and disruption of speech and chewing are reduced. An additional consideration when choosing a clear aligner to straighten anterior teeth is its improved appearance. Despite this aesthetic benefit, biomechanical restrictions exist. Clear aligners make it difficult to control root position, thus bonded attachments to the teeth and adjustments to the aligners are required to achieve a number of significant forms of tooth movement.4
The gingival horizontal length can be lengthened or the T-loop can be made as long as it can be in an apical direction to achieve greater M/F ratios. 23
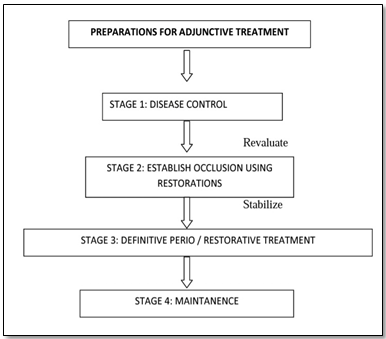
Adjunctive Orthodontic Treatment Sequence
The process for treating patients who need supplementary orthodontic treatment, only when disease control has been achieved can orthodontics be utilized to establish occlusion, and the occlusion should be stabilized before using definitive restorative treatments.
Procedures for Adjunctive Orthodontic Treatment
The following procedures are frequently used as part of adjunctive treatment:
Repositioning of teeth that have shifted due to extractions or bone loss in order to provide room for implants or fixed or removable partial dentures.
Cross-bite correction if it affects jaw function.
Forced eruption of severely damaged teeth to reveal healthy root structure for crown placement.
Correct anterior tooth alignment for successful splinting or more aesthetically pleasing restorations.
Discussion on Adjunctive Orthodontic Treatment Procedures
Uprighting posterior teeth
Uprighting posterior teeth is one of the pre-prosthetic adjunctive orthodontic procedures. The surrounding teeth typically tip and rotate toward the extraction space when a posterior tooth is gone. A pseudo pocket that may be difficult for the patient to cleazn develops as the teeth shift.
The second and third molars should be uprighted together if the third molar is available. Tip the second molar crown to create a space for prosthetic restoration, or mesially drift the root to close the space. There are several techniques for uprighting posterior teeth like - Fixed appliance technique for uprighting one molar with a Continuous flexible wire, an Auxiliary spring, T-loop spring, a Compressed coil spring etc.
Crossbite Correction
Crossbite elastics were used to correct crossbite. Cross-elastics, also known as "through the bite" pressures, extrude teeth while moving them buccolingually. Adults with posterior crossbite should be careful when using these elastics to prevent excessive anterior opening of the bite. Rarely is a cross-elastic recommended for an anterior crossbite.4
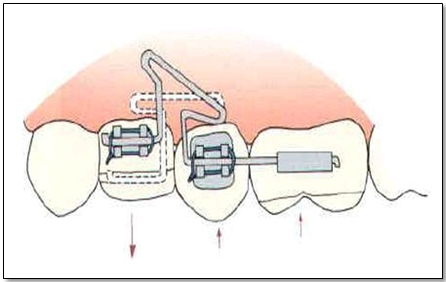
Extrusion (Forced eruption)
Ingber first developed orthodontic extrusion of teeth, or so-called "forced eruption," in 1974 for the treatment of one-wall and two-wall bony pockets that were challenging to cure with conventional therapy alone. The bone defect is smoothed out as a result of the extrusive tooth movement, which places the intact connective tissue attachment coronally.24 Forced eruptions may be necessary to increase the clinical crown length of single teeth, repair intraosseous abnormalities, and treat root fractures. Whether a tooth should be removed or forced to erupt is decided by six factors - Root length, Root morphology, Fracture level, Relative tooth importance, Aesthetics, and Endo/Perio prognosis are a few of them.25
There are various methods for forcing a tooth to erupt, such as bonding a stabilizing wire made of 19 x 25 steel to the facial surfaces of neighbouring teeth. Between the stabilizing wire and a pin inserted directly into the crown of the tooth to be extruded, an elastomeric module is stretched. T-loop segments on a rectangular wire (Figure 4). The desired extrusive force is produced by a continuous orthodontic wire that has been triggered.4
Alignment of Anterior Teeth
Preparation for buildups, veneers, or implants to improve the appearance of the maxillary incisor teeth is the main reason for supplementary orthodontic treatment to rectify misaligned anterior teeth. A maxillary central diastema is the most common issue, which is frequently made worse by irregular spacing brought on by undersized or absent lateral incisors. When the alignment of the lower incisors is taken into account to allow for restorative access, improve occlusion, or allow the patient to preserve the teeth, crowding is typically the issue.
Retention and Stability Considerations for Adult Patients
Special measures should be taken when contemplating retention in patients who are adults:
Before removing the appliance, root parallelism must be radiographically confirmed.
Clinical evaluation should be done when focal relation and habitual occlusion coexist.
Incisal guidance ought to be managed medically or with mounted models.
Joint symptoms need to be evaluated.
Patients should express their worries.
Retention and restorative therapy timing have to be synchronized.
Clinical and radiographic procedures should be used to control periodontal disease.
8. Prior to retention, the original malocclusion should be assessed.26
The treatment strategy should include retention mechanisms. The original abnormality, amount and type of treatment, treatment outcome, periodontal state, interdisciplinary treatment strategy, and several etiologic factors all affect how long the retention phase lasts. Depending on the type of therapy, retention planning is classified into three categories: semi-permanent or permanent retention, limited retention in terms of type and time, and no retention. The level of the marginal periodontium and the state of the teeth are significant determinants of the kind of retention. Fixed retention, surgical techniques, or removable retainers may be preferred.26
Essix retainers, Hawley retainers, positioners, fixed retention appliances (lingual retainer), and fiber retainers are examples of retention appliances. 26
Conclusion
A lot of individuals have malocclusions that can be fixed with either adjunctive or full orthodontic treatment. The orthodontist should be willing to treat adults, carefully assess the patient's expectations, and co-operate with them. However, the patient must have a thorough evaluation for systemic illnesses, perio-restorative issues, root resorption, and temporomandibular joint disorders before beginning treatment. Before beginning orthodontic therapy, all systemic and oral illnesses should be effectively addressed and managed. By participating in the interdisciplinary treatment strategy, both the orthodontist and the patient would be pleased with the results of the cosmetic and functional rehabilitation.