Introduction
Relapse is an unwanted outcome after orthodontic treatment, and one of the most common conditions being “Midline Diastema”. The relapse of the maxillary diastema after orthodontic space closure might be as great as 50%.1 There are many options available for correction of midline diastema in literature.2 Here, we suggest a relatively fast and effective way of closure of the relapsed diastema.
Case Report and Treatment
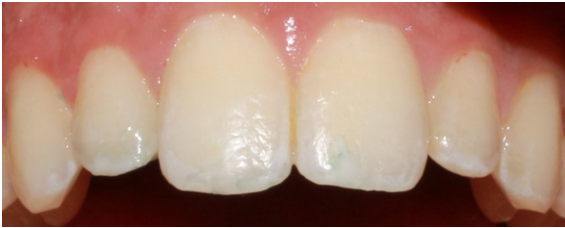
The patient had received orthodontic treatment with extraction of all 1st premolars. The retainer in the upper arch broke leading to a midline diastema. At the clinical examination, a good Class I interarch relationship was observed. A 2mm diastema was noticed between the maxillary central incisors (Figure 1). The patient did not want fixed appliances on labial side of the teeth. Hence, he was presented with a treatment option which involves bonding of Begg brackets on the lingual aspect of upper anterior teeth (Figure 3).
Figure 2
a) Periapical radiograph with noticeable amount of root resorption before orthodontic treatment. b) Periapical radiograph after closure of midline diastema.

Procedure
Oral prophylaxis of the lingual surfaces of upper four anterior teeth was done to remove any debris or calculus.
Four contoured Begg brackets were placed on the lingual surfaces of the upper anterior teeth in center of the crown following regular bonding protocols.
Coloured restorative composite was placed on occlusal surfaces of Maxillary 1st Molars to raise the bite.
Spaced E-chain of four modules length was stretched and engaged (Figure 3 d) in the Begg brackets. At the end of the month it was observed that the diastema has closed and there was minimal mobility in the teeth (Figure 4). After closure of the midline diastema retention protocols were followed (Figure 5). Bonded retainers which are well accepted by patients and relatively independent of patient cooperation were given.
Discussion
Diastemas are spaces or gaps between two or more consecutive teeth. The present case is an example of midline diastema occurring after orthodontic treatment. On intraoral examination it was observed that the two central incisors showed a gap of 2mm which increased from gingival to occlusal direction. The maxillary central incisors showed vital signs, minimal mobility and no signs of discolouration. On radiographic examination (Figure 2 a) there was notable amount root resorption present this could be attributed to the retraction and intrusion forces applied during the first orthodontic treatment.
The patient had already been through orthodontic treatment, and did not want appliances on the labial side. The diastema needed correction for esthetic reasons hence, the present option of placing appliance on the lingual side of the anterior teeth was suggested.
David Lee Mitchell3 in his study placed tube-type M brackets on upper central incisors, and edgewise M brackets on upper central incisors of two different patients respectively as both of them had central incisor’s diastema that required closing. An 0.016-inch round sectional archwire was placed between these brackets, and the ends were bent back to prevent them from slipping out of the brackets. A force of 3 oz was applied by elastic placed from the distal side of one bracket to the distal side of the other bracket. Both the patients required about 1 month of force to close the diastema.
In the present case report Begg brackets were placed on the lingual side of the upper anterior teeth rather than the labial side as done by Mitchell in his article for esthetic reasons. Begg brackets were placed on the lingual side of the lateral incisors in addition to central incisors to avoid unwanted redistribution of spaces. Placing the brackets on the lingual side of the anterior teeth may cause frequent bond failure because of the incisor edges of the lower anterior teeth during the process mastication. To avoid this, bite was raised by placing coloured composite on the upper 1st Molars. Placing coloured composite also helps during the process of debonding by reducing the amount of tooth structure while removing the adhesive. Instead of elastics and sectional wire spaced or Long E-chain was engaged to the brackets. The diastema was closed in 1 month’s time similar to that of the two cases as shown by Mitchell in his article. The amount of root resorption was minimal on comparison with pre treatment radiograph, and this was evident in the radiographs taken after space closure (Figure 2 b). To avoid relapse bonded retainer was placed on the four anterior teeth in cervical third to prevent interference from the mandibular incisors and breakage.
Conclusion
The present method is a less time consuming, one of the effective way of closing relapsed midline diastema in less period of time.
Ethics Approval and Consent to Participate
The treatment was done by taking approval from both patient and parent. The patient was explained regarding pros and cons of the treatment.