- Visibility 87 Views
- Downloads 20 Downloads
- DOI 10.18231/j.jco.2023.006
-
CrossMark
- Citation
Evaluation of shear peel bond strength and fatigue stress of different orthodontic banding cements – An in vitro study
Introduction
The use of Stainless steel Bands for orthodontic attachment remains vital for the management of orthodontic case despite the progression of acid etch composite technique.[1] Despite the increased popularity of bonding, about 85% of the orthodontists prefer to band the posterior teeth (Gottlieb et al., 1986).[2] Banding offers more reliability due to better resistance to occlusal interferences.[3] As the molar band undergoes more tensile and shear force, good retention is necessary which depends on the close fit of the band to the tooth and on chemical adhesion provided by the cement.[4], [5] Early band loss is associated with time-consuming recementation of the band and also loosening of the band bears the risk of demineralization.[6] The luting cements used should produce sufficient bond strength between enamel, cement and orthodontic band to avoid any loosening of the bands.
For the past few decades, zinc phosphate cements were used widely for band cementation, but intraorally these cements have high solubility and mechanical adhesion is much-needed for their retentive effect.[7], [8] On the other side, Polycarboxylate cements react chemically with enamel and stainless steel but these cements have increased viscosity, high solubility and reduced setting time.[9]
Glass ionomer cements have become the most commonly used cement for band cementation, due to fluoride release and uptake, microbial inhibition, and adhesion to both enamel and metal. The main disadvantages of glass ionomers are that it need up to 24 hours to reach maximum strength and also its vulnerability to moisture contamination during the setting reaction.[10] GICs have superior tensile and compressive strengths and a lower failure rate clinically compared with other cements (Norris et al., 1986; Durning, 1994; Stirrups,1991.[10], [11], [12]
Millett and his associates found that the clinical failure rate of bands cemented on natural teeth with glass ionomer cement (GIC) ranged from 6% to 26% over observation periods ranging from 12 to 24 months.[13] Various studies of force values required to remove cemented bands from the teeth show that RMGIC and GIC are generally equivalent, whereas fatigue studies show RMGIC has superior fatigue properties.[14]
Adhesive Remnant Index by Artun and Bergland (1984) was used to evaluate the amount of adhesive left on the tooth after debracketing.[15] Currently, Modification of ARI is used to evaluate the amount of cement left on the tooth after debanding.[16] Several studies showed that the site of cement failure of GIC is more common at the band-cement interface while some studies showed that it is more common at the cement-enamel interface.[17]
The principle of ball milling as used in mineral processing can be applied in dentistry investigative procedures to produce mechanical fatigue, thereby simulating the oral forces. The present study attempts to provide necessary information to the orthodontist towards careful selection of the cements with good bond strength for orthodontic banding and aid in the improvement of the orthodontic treatment.
Materials and Methods
This study was conducted in the Department of Orthodontics and Dentofacial Orthopedics, KSR Institute of dental science and Research, Tiruchengode, Namakkal district on approval from Institutional Review Board and Institutional Ethical Committee (IEC approval code 210/KSRIDSR/EC/2018). The physical tests were performed at Sona College of Technology, Salem, Tamilnadu and PSG Institute of Technology and Applied Research, Coimbatore, Tamilnadu. Freshly extracted mandibular second molars which were caries- free and without restorations or surface abnormalities were included in the study. The samples were divided into four groups Group A - Medicept dental Xtralute radiopaque glass ionomer luting cement, Group B – Voco Meron glass ionomer luting cement, Group C - GC Fuji Ortho band paste pak glass ionomer orthodontic band cement, Group D – Prevest denpro Micron luting glass ionomer luting cement. One hundred and twenty caries-free extracted human mandibular second molar teeth were used in this study out of which eighty molar teeth were used to assess the shear peel bond strength and other forty molar teeth were used to study the fatigue survival time. The collected teeth were stored in distilled water continuously after extraction. These samples were randomly divided into four groups of twenty each for the retentive strength study group. Each of the eighty teeth was mounted vertically in a self-cure acrylic resin so that the crown was exposed for banding and also all the four groups are colour coded for easier identification ([Figure 1]). The teeth were then cleaned with pumice, washed in distilled water, and dried in a stream of air. Stainless steel orthodontic bands with no attachments were fitted and seated around the teeth including adaptation of the margins with a band seater. A 1 mm stainless steel wire was attached to the mid- buccal and mid-lingual sides of the band with hard solder to aid in the loading of the specimen in the universal testing machine ([Figure 2]). Soldering of the stainless steel loop was done with the help of the working model after recording the impression of the specimens. The bands were selected and placed by the same operator in order to eliminate any operator bias in band positioning and fitting. The bands were adapted to each tooth and the bands were cemented with cements according to manufacturer’s instructions. The Specimens were then transferred to store at 37°C for 24 hours, and they were subsequently tested for retentive strength.
Shear peel bond strength evaluation
To determine the SPBS, each specimen was secured in a universal testing machine with the crosshead speed of 1mm/minute by means of 1 mm stainless steel loop attached to the buccal and lingual surfaces of the band. Testing was continued until the band was fully removed from the teeth. The maximum force needed to completely remove the band from the teeth was measured in Newtons. The band was then cleaned and cut with band cutting scissor, and laid out flat such that its length and width were measured to the nearest 10th of a millimeter with millimeter caliper, and thus, its area was determined in mm.[2] The Shear peel bond strength was calculated by dividing the peak load value by band area (1 MPa = 1 N/mm2).
Adhesive remnant index
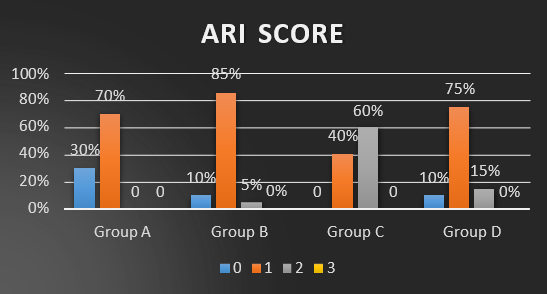
The ARI score given by Artun and Bergland was as follows 0 - No cement remains on the tooth surface, 1 - less than half the crown surface under the band is covered by cement, 2 - more than half the crown surface under the band is covered by cement, 3 - the entire crown surface under the band is covered by cement.


Survival Time Evaluation
Forty human mandibular teeth were used to test the survival time of the bands for different cements. The samples were coded by diamond bur at the root surface of the teeth and were also colour coded for each cement group. Then the bands were cemented according to the manufacturer’s instructions and transferred to store at 370c for 24 hours. The samples were then transferred to ball mill machine. The ball mill contains spheres and distilled water at 370c, rotating at 100 revolutions per minute. After every hour of testing, those samples with loose bands were removed. Fresh distilled water was replaced after every hour of inspection.
Statistical Analysis
The data collected were compiled using MS-Office Excel and was subjected to Statistical analysis using IBM corp. SPSS (Statistical package for social sciences) Statistics for windows, version 20.0 (Armonk, NY). Descriptive and inferential statistics were used to analyze the data. Normality of the data was assessed. Kruskal Wallis Test was done to compare the shear peel bond strength. Survival analysis was done using Kaplan–Meier model to calculate the mean survival rate of the bands.
Results
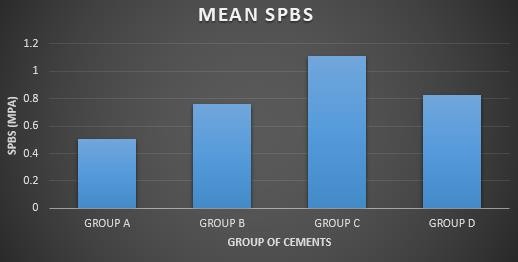
The resultant data obtained after statistical analysis were further analyzed and tabulated. The distribution and comparison of mean shear peel bond strength among the four groups are given in [Table 1]. The mean shear peel bond strength of the bands cemented with Group C (1.1 MPa) was greater than that of those bonded with Group A (0.5 MPa), B (0.7 MPa) and D (0.8MPa). The mean SPBS of group D was greater when compared with group A and B. Among groups A and B, mean SPBS of group B was greater than group A.
|
Groups |
Minimum |
Maximum |
Mean |
Std. Deviation |
P. Value |
|
Group A |
.0030 |
1.0118 |
.506730 |
.3250328 |
< 0.001 |
|
Group B |
.1685 |
1.7400 |
.760185 |
.3734846 |
|
|
Group C |
.2463 |
1.8160 |
1.106845 |
.4133019 |
|
|
Group D |
.0749 |
1.4975 |
.828810 |
.3561922 |
The ARI scores frequency and percentage in each of the four groups are given in [Table 2]. The Bands cemented with Group A, Group B and Group D showed a higher frequency of ARI score of 1 indicating that that less than half of the crown surface under the band was covered by the cement. The Bands cemented with Group C showed a higher frequency of ARI score of 2 indicating that more than half of the crown surface under the band was covered by the cement.
|
|
ARI Score |
P Value |
||
|
Groups |
|
Frequency |
Percent |
|
|
A |
0 |
6 |
30.0 |
< 0.001 |
|
1.0 |
14 |
70.0 |
||
|
2.0 |
0 |
0 |
||
|
3.0 |
0 |
0 |
||
|
B |
0 |
2 |
10.0 |
|
|
1.0 |
17 |
85.0 |
||
|
2.0 |
1 |
5.0 |
||
|
3.0 |
0 |
0 |
||
|
C |
0 |
0 |
0 |
|
|
1.0 |
8 |
40.0 |
||
|
2.0 |
12 |
60.0 |
||
|
3.0 |
0 |
0 |
||
|
D |
0 |
2 |
10.0 |
|
|
1.0 |
15 |
75.0 |
||
|
2.0 |
3 |
15.0 |
||
|
3.0 |
0 |
0 |
An overall assessment shows that GC Fuji Ortho band paste pak orthodontic band cement (Group C) had greater mean shear peel bond strength and survival time among all the groups used in this study.
Discussion
Generally, the band cemented with the material which has more tensile strength require greater force to deband from the tooth. The band failure mainly occurs due to the mechanical stress on the band-tooth interface (Smith, 1983).[18]
Glass ionomer cements provide superior clinical performance due to reduction in the failure of the bands (Fricker and Mclachlon, 1985, 1987; Mizrahi, 1988; Stirrups, 1991).[19], [20]
The glass ionomer luting cements Medicept dental Xtralute radiopaque (Group A), Voco Meron glass ionomer luting cement (Group B), GC Fuji ortho band paste pak (Group C) and prevest denpro Micron luting glass ionomer luting cement (Group D) were chosen for this study as these cements are the most commonly preferred cements by the orthodontists. For each cement group, 20 human molars were used for Shear peel bond strength testing. This sample size is optimal for the studies of this nature and storage of the specimens also complied with the guidelines in the orthodontic literature (Fox, 1994).[21]
In this study, the mean shear peel bond strength differed significantly between the cement groups.
The mean shear peel bond strength of the bands cemented with GC Fuji Ortho band paste pak orthodontic banding cement (Group C) was significantly greater among the four groups.
This may be attributed to the easier, convenient handling characteristics and predetermined mixing ratio given by the dispenser leading to the homogenous mix. There was no statistically significant differences among the other three groups. However the mean shear peel bond strength of the bands cemented with Group D was greater than that of those bonded with Group A and Group B. Also the mean shear peel bond strength of the bands cemented with Group B was greater than that of those bonded with Group A. The findings in this study is in agreement with the previous studies done by Sfondrini and his associates (Sfondrini et al., 2010).[16] A previous experiment conducted by millet and associates also found statistically significant difference between Transbond Plus and ketac cem cements in which ketac cem had greater retentive strength (Millet et al.,2003).[13] In contrast to that, another study done by millet and his associates found no significant differences in shear-peel bond strength of bands cemented with 3M Multi-Cure and Ketac-Cem(Millet et al.,2003)[22]and also Aggarwal and collegues found no significant difference in mean shear-peel bond strengths between 3M Multi-Cure and Transbond Plus(Aggarwal et al.,2000).[23] Herion and his associates also did not find differences in bond strength when comparing the Transbond plus with both Ketac-Cem and 3M Multi-Cure in one of their studies(Herion et al.,2007).[22] The cements used in this study were not compared previously but similar products were assessed. Although most of the experimental protocol in this study was similar to that of previous studies, our numerical findings cannot be easily compared with those of previous studies for several reasons.[24], [25] First, there were different band removal mechanisms and also the bands tested were different in those studies.
Second, comparisons with previous studies was difficult because different cements were used and the intent of this study was to compare the most commonly used orthodontic luting cements for improved handling characteristics and good bond strength.
In this study the amount of cement remaining on the tooth after debanding differed significantly for the bands cemented with all the groups and bond failure occurred predominantly at the enamel-cement interface. The bands cemented with GC Fuji ortho band paste pak orthodontic banding cement (Group C) showed a higher frequency of ARI score of 2 indicating that more than half of the crown surface under the band was covered by the cement. This was in agreement with the previous studies by sfondrini et al., 2010; millet et al. and cantekin et al., 2014. Previous studies that evaluated the site of cement failure of GICs showed conflicting results.[26] In those studies, the site of cement failure was shown to occur primarily at the band-cement interface with GIC, whereas failure was more common at the enamel-cement interface for RMGIC and compomers.[26] The differences in the results of the present study may be due to the differences in methodologies when compared with some of the studies. For example, we have used human molars instead of porcelain or gold crowns,[22] different band removal mechanism,[23] specimen storage system,[24] a different debanding location evaluation scale and crosshead speed which were changed in the previous studies.[17]
In this study, the survival time of the bands cemented with GC Fuji ortho band paste pak orthodontic banding cement (Group C) was greater than those bands banded with Medicept dental Xtralute glass ionomer luting cement (Group A), Prevest Denpro micron luting glass ionmer cement (Group D) and Voco Meron glass ionomer luting cement (Group B). The findings of this study was consistent with a study done by Herion (Herion et al. 2007).[22] However, Millett et al. compared transbond plus with Ketac-Cem for orthodontic band cementation, and they found no statistically significant difference in survival times among the adhesive cements (Millett et al. 2003). Another study done by millett and his associates was also in agreement with our findings(Millet et al., 2003). It is possible that survival time could be improved if GIC were tested after greater time interval than the 24-hour interval where the added time may allow for further setting.[27] A p rospective clinical trial would be ideal for comparing the cements and its efficient usage for orthodontic case management.
An overall assessment shows that GC Fuji Ortho band paste pak orthodontic band cement (Group C) had greater mean shear peel bond strength and survival time among all the groups used in this study. Though the present study helps the orthodontist towards careful selection of the cements with good bond strength for orthodontic banding, further studies are recommended on patients to aid in the successful orthodontic management.
Conclusion
The following conclusion were drawn from the present study:
GC Fuji ortho band paste pak orthodontic banding cement required significantly higher forces to deband in comparison with Medicept dental Xtralute radiopaque glass ionomer luting cement, Prevest Denpro micron luting glass ionmer cement and Voco Meron glass ionomer luting cement.
Bond failure occurred predominantly at the enamel-cement interface.
The survival time of the bands cemented with GC Fuji ortho band paste pak orthodontic banding cement was greater than those bands banded with Medicept dental Xtralute radiopaque glass ionomer luting cement, Prevest Denpro micron luting glass ionomer cement, and Voco Meron glass ionomer luting cement.
Source of Funding
None.
Conflict of Interest
None.
References
- P Durning, JF Mccabe, PH Gordon. A laboratory investigation into cements used to retain orthodontic bands. Br J Orthod 1994. [Google Scholar]
- EH Gottlieb, AH Nelson, D Vogels. JCO study of orthodontic diagnosis and treatment procedures. J Clin Orthod 1996. [Google Scholar]
- DT Millett, A Cummings, S Letters, E Roger, J Love. Resin-modified glass ionomer, modified composite or conventional glass ionomer for band cementation? - An in vitro evaluation. Eur J Orthod 2003. [Google Scholar]
- JD Williams, ML Swartz, RW Phillips. Retention of orthodontic bands as influenced by the cementing media. Angle Orthod 1965. [Google Scholar]
- AD Wilson, BE Kent. A new translucent cement for dentistry. The glass ionomer cement. Br Dent J 1972. [Google Scholar]
- E Mizrahi. Retention of the Conventional Orthodontic Band. Br J Orthod 1977. [Google Scholar]
- P Hotz, JW Mclean, I Sced, AD Wilson. The bonding of glass ionomer cements to metal and tooth substrates. Br Dent J 1977. [Google Scholar]
- E Kvam, J Broch, IH Nissen-Meyer. Comparison between a zinc phosphate cement and a glass ionomer cement for cementation of orthodontic bands. Eur J Orthod 1983. [Google Scholar]
- D Brown. Orthodontic materials update-orthodontic band cements. Br J Orthod 1989. [Google Scholar]
- AD Wilson, JM Paddon, S Crisp. The hydration of dental cements. J Dent Res 1979. [Google Scholar]
- DR Stirrups. A comparative clinical trial of a glass ionomer and a zinc phosphate cement for securing orthodontic bands. Br J Orthod 1991. [Google Scholar]
- P Durning, JF Mccabe, PH Gordon. A laboratory investigation into cements used to retain orthodontic bands. Br J Orthod 1994. [Google Scholar]
- DT Millett, S Duff, L Morrison, A Cummings, WH Gilmour. In vitro comparison of orthodontic band cements. Am J Orthod Dentofac Orthop 2003. [Google Scholar]
- JP Fricker. A 12-month clinical comparison of resin-modified light activated adhesives for the cementation of orthodontic molar bands. Am J Orthod Dentofac Orthop 1997. [Google Scholar]
- J Artun, S Bergland. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod 1984. [Google Scholar]
- MF Sfondrini, V Cacciafesta, E Noga, A Scribante, C Klersy. In Vitro Bond Strength of Four Orthodontic cements. J Adhes Dent 2010. [Google Scholar]
- K Cantekin, E Delikan, S Cetin. In vitro bond strength and fatigue stress test evaluation of different adhesive cements used for fixed space maintainer cementation. Eur J Dent 2014. [Google Scholar]
- DC Smith. Dental cements-Current status and future properties. Dent Clin North Am 1983. [Google Scholar]
- E Mizrahi. Glass ionomer cements in orthodontics- An update. Am J orthod Dentofac orthop 1988. [Google Scholar]
- JP Fricker, MD Mclachlan. Clinical studies of glass ionomer cements. Part I--A twelve month clinical study comparing zinc phosphate cement to glass ionomer. Aust Orthod J 1985. [Google Scholar]
- NA Fox, JF Mccabe, JG Buckley. A critique of bond strength testing in orthodontics. Br J Orthod 1994. [Google Scholar]
- T Herion, JL Ferracane, DA Covell. Three cements used for orthodontic banding of porcelain molars. Angle Orthod 2007. [Google Scholar]
- M Aggarwal, TF Foley, D Rix. A comparison of shear-peel band strengths of 5 orthodontic cements. Angle Orthod 2000. [Google Scholar]
- R Maijer, DC Smith. A comparison between zinc phosphate and glass ionomer cement in orthodontics. Am J Orthod Dentofac Orthop 1988. [Google Scholar]
- DT Millett, PH Gordon. The performance of first molar orthodontic bands cemented with glass ionomer cement. Br J Orthod 1992. [Google Scholar]
- TJ Gillgrass, PC Benington, DT Millett, J Newell, WH Gilmour. Modified composite or conventional glass ionomer for band cementation? A comparative clinical trial. Am J Orthod Dentofac Orthop 2001. [Google Scholar]
- U Lohbauer, R Frankenberger, N Kramer, A Petschelt. Time-dependent strength and fatigue resistance of dental direct restorative materials. J Mater Sci Mater Med 2003. [Google Scholar]
How to Cite This Article
Vancouver
M AK, S R, A R, K P, N. RP, S R. Evaluation of shear peel bond strength and fatigue stress of different orthodontic banding cements – An in vitro study [Internet]. J Contemp Orthod. 2025 [cited 2025 Sep 08];7(1):30-35. Available from: https://doi.org/10.18231/j.jco.2023.006
APA
M, A. K., S, R., A, R., K, P., N., R. P., S, R. (2025). Evaluation of shear peel bond strength and fatigue stress of different orthodontic banding cements – An in vitro study. J Contemp Orthod, 7(1), 30-35. https://doi.org/10.18231/j.jco.2023.006
MLA
M, Ajith Kumar, S, Raja, A, Raja, K, Prabhakar, N., Rehna Parvin, S, Revathy. "Evaluation of shear peel bond strength and fatigue stress of different orthodontic banding cements – An in vitro study." J Contemp Orthod, vol. 7, no. 1, 2025, pp. 30-35. https://doi.org/10.18231/j.jco.2023.006
Chicago
M, A. K., S, R., A, R., K, P., N., R. P., S, R.. "Evaluation of shear peel bond strength and fatigue stress of different orthodontic banding cements – An in vitro study." J Contemp Orthod 7, no. 1 (2025): 30-35. https://doi.org/10.18231/j.jco.2023.006
