- Visibility 396 Views
- Downloads 49 Downloads
- Permissions
- DOI 10.18231/j.jco.2023.009
-
CrossMark
- Citation
Idiopathic osteosclerosis in a Class III patient treated with facemask therapy and hybrid hyrax- A case report
Abstract
Class III malocclusion is the most common form of malocclusion requiring orthognathic surgery. Hence, early diagnosis and intervention is often beneficial in reducing the severity of the problem. Protraction of the maxilla using a facemask accompanied by rapid maxillary expansion (RME) is the ideal treatment option for growing patients with Class III malocclusion and deficient maxilla. Idiopathic osteosclerosis is an asymptomatic, benign lesion that usually develops early in life. Its origin could be associated to reaction to inflammation or occlusal trauma, occurring at the time of teeth transition. Here, in this case report, we have showed the successful management of a Class III adolescent patient, diagnosed with idiopathic osteosclerosis, with face mask therapy and hybrid hyrax expansion appliance following Alt-RAMEC protocol. Also, we have showed the management of disturbed wound healing which might occur after palatal implant removal.
Introduction
The prevalence of Class III malocclusion varies greatly in different populations. Compared to other regions, Indian population shows the lowest prevalence of 1.19%. Among children aged 5-15 years, the prevalence was reported to be 0–4.76%.[1] Class III malocclusion is the most common form of malocclusion requiring orthognathic surgery. Hence, early diagnosis and intervention is often beneficial in reducing the severity of the problem and eliminating the need for procedures in the future.
Many treatment approaches for growing Class III malocclusion patients are found in the literature, including intraoral and extraoral appliances such as a face-mask, chin cap, functional regulator-3, Class III elastics, etc. McNamara suggested that rapid maxillary expansion, when used with face mask, may enhance maxillary protraction in Class III patients with maxillary deficiency.[2] Liou and Tsai introduced the Alt-RAMEC protocol, an expansion and constriction protocol that could be used for achieving greater maxillary protraction by distraction of the circum-maxillary sutures.[3]
A study, conducted by Yilmaz et al., reported that the expansion and constriction protocol for maxillary expansion resulted in forward maxilla protraction.[4] Hence, in recent years, rapid maxillary expansion along with face mask for protraction of the maxilla has become a standard protocol in the treatment of Class III growing patients with maxillary deficiency. Proper case selection and prolonged treatment with long-term follow-up is essential for a successful orthopaedic growth modification.
Idiopathic osteosclerosis (IO) is defined as an asymptomatic, benign and radiopaque lesion. The biological behaviour of IO is not fully known. Proper diagnosis of idiopathic osteosclerosis from other radiopaque lesions is essential for proper management.[5]
This case report describes the successful treatment of an adolescent male patient with skeletal Class III malocclusion using facemask therapy and hybrid hyrax expansion appliance, following the Alt-RAMEC protocol. The patient was later on diagnosed with idiopathic osteosclerosis.
Diagnosis and Treatment Plan

A 12-year-old male reported with the complaint of backwardly placed upper front teeth. There was no relevant past medical or dental history. Also, no abnormal habits were present. Extra oral examination revealed a straight facial profile, mesoprosopic facial type, no apparent facial asymmetry, increased lower facial third, slightly deficient maxillary projection and lower lip positioned ahead of upper lip. Intraorally, there was anterior cross bite present, with reverse overjet of 1mm and reverse overbite of 2 mm. Canine relationship was Class I on the right, and Class III on the left. Molar relationship was super Class I on the right and Class III on the left. Dental midline was deviated 2 mm to the right. Occlusal caries was present i.r.t. maxillary and mandibular permanent first molars (16, 26, 36, 46) ([Figure 1]). All functional examinations were normal.
Radiographic examination revealed that all third molars were present, with root formation remaining. Hand wrist radiograph and maturation stage of the cervical vertebrae (CS1) revealed a significant amount of growth remaining. Lateral cephalometric evaluation revealed a Class III skeletal base (ANB, - 30, Wits appraisal, -5mm) with retroclined lower incisors (L1 to N-B, 17°/2mm).
Treatment objectives
Correction of anterior crossbite.
Improvement of the skeletal jaw relationship.
Achieve Class I molar relationship bilaterally.
Achieve normal overjet and overbite.
Correct the dental midline discrepancy.
Obtain a harmonious soft tissue profile.
Treatment options
The first treatment option was aimed at correction of the skeletal discrepancy in the maxilla-mandibular relationship by the use of a face-mask and a skeletally anchored hybrid-hyrax for maxillary protraction.
The second option was treatment with orthodontic fixed appliances and potential orthognathic surgery carried out in the future.
The first treatment plan needed strong patient compliance to achieve treatment success. The patient’s guardians were informed of it, and advised that unpredictable growth of the mandible could create the need for an intervention with orthognathic surgery during adulthood. Also, the patient’s guardians were explained the pros and cons of both the approaches.
The patient’s family agreed to the first treatment approach, with no extractions done to keep a future scope of orthognathic surgery if needed.
Treatment progress
Treatment was initiated with a posterior bite plate placed in the lower arch, and bonding in the upper arch using a pre adjusted edgewise fixed appliance (0.022′′x0.028′′ slot, 3M Unitek) with MBT prescription. Leveling and alignment was initiated in the upper arch with 0.014′′ NiTi, and continued with 0.016′′ NiTi and 0.016′′×0.022′′ NiTi (3M Unitek nitinol super elastic, USA). After sufficient leveling and alignment in the upper arch, the lower arch was bonded. The posterior bite plate was transferred to the upper arch to facilitate leveling and alignment in the lower arch.
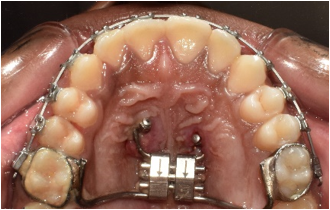
After the leveling and alignment period, treatment had to be halted, due to Covid-19 and the patient being unable to come for appointments due to travel issues. After 18 months, treatment resumed with the placement of hybrid hyrax, for disarticulating the circummaxillary sutures to facilitate maxillary protraction. The Hyrax was placed at the mid palatine rugae, with its buccal arms extending anteriorly to the first premolar region and the posterior arms were welded to bands on the first permanent molars (16 and 26). The anterior arms of the hyrax consisted of two rings at the anterior palatal region for the insertion of mini-implants. Under local anaesthesia, two mini-implants (SK Surgicals) (2 mm diameter, 10 mm length) were inserted, at the level of the second and third palatal rugae, adjacent to the midline suture.([Figure 2])
The Alt-RAMEC protocol was used for activation. The hyrax was activated for expansion with a 180° rotation, twice a day, resulting in a daily activation of 0.8mm. One week of expansion of the screw was followed by a week of compression, this sequence was continued for 9 weeks.[6], [7]
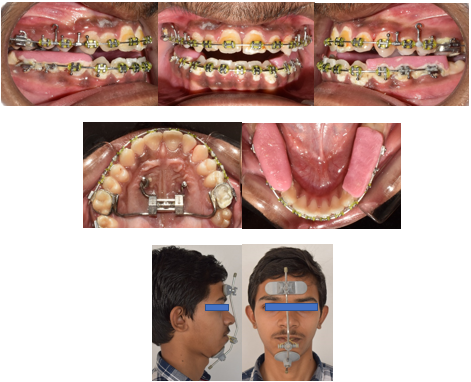
At the same time, face mask therapy was started. Elastics were engaged from the face mask to hooks of 8mm on 0.019″×0.025″ Stainless steel arch wire (SS American Orthodontics) on the upper arch,[8] placed between the first and second premolars on both sides, and engaged 25 degrees of inclination to the occlusal plane. Initially, at the time of delivery, 3/8″, 8 oz elastics was used. After two weeks, it was changed to 1/2″, 14oz, and, progressively, increased to 5/16″, 14 oz to obtain an orthopaedic force of 400gm per side. The elastics were used in a cross-over fashion so as to minimise the risk of lacerations to the corner of the mouth. The face mask was advised to be worn 16 hours daily with strict compliance.[9]
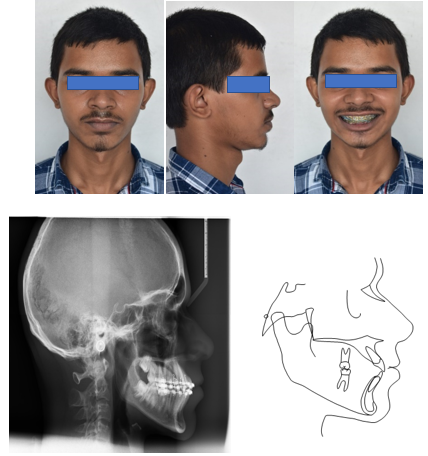
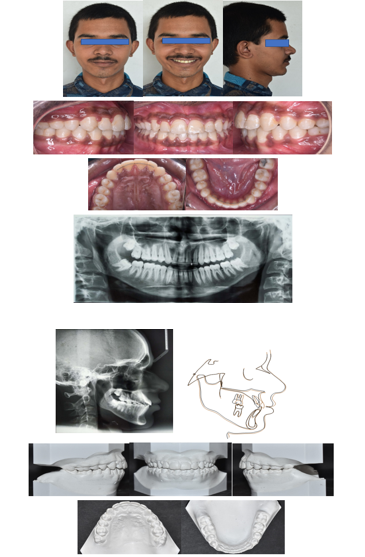
After, nine months of face mask therapy,[9] a satisfactory relationship in the anteroposterior plane was observed, along with positive changes in the patient’s profile.([Figure 3]) The posterior bite plates were removed. Treatment was continued with the use of cross elastics (3/16′′, 4.5 oz), on 0.019′′X0.025′′ Stainless steel archwire (SS American Orthodontics), for the correcting the midline deviation.
After three months, continuous e-chain was used in the lower arch for closing the residual spaces. 0.014′′ Nickel Titanium archwire (3M Unitek nitinol super elastic, USA) was used for settling in both the arches. After debonding, fixed retainers were bonded in both upper (2-2) and lower arches (3-3). Total treatment time was 40 months.
|
Sl. No |
Measurements |
Range |
|
Actual |
|
|
Pre-treatment |
Mid-treatment |
Post-treatment |
|||
|
1 |
SNA |
82˚ |
80˚ |
84˚ |
84˚ |
|
2 |
SNB |
80˚ |
83˚ |
83˚ |
83˚ |
|
3 |
ANB |
2˚ |
-3˚ |
1˚ |
1˚ |
|
4 |
Wits appraisal |
-2 – 4mm |
-5mm |
3mm |
3mm |
|
5 |
U I to N-A(mm) |
4mm |
2.5mm |
7mm |
5.5 mm |
|
6 |
U I to N-A(angle) |
22˚ |
24˚ |
32˚ |
28˚ |
|
7 |
L I to N-B (mm) |
4mm |
2mm |
5 mm |
4 mm |
|
8 |
L I to N-B (angle) |
25˚ |
17 ˚ |
28˚ |
25˚ |
|
9 |
U I to LI (Interincisal -angle) |
131˚ |
148˚ |
117˚ |
125 ˚ |
|
10 |
Upper incisor to S-N plane |
102˚ ± 20 |
104˚ |
121˚ |
122˚ |
|
11 |
IMPA (Incisor mandibular plane angle) |
90˚ |
75˚ |
89˚ |
84˚ |
|
12 |
Upper lip to S-line |
0-2 mm |
-1mm |
1.5mm |
2mm |
|
13 |
Lower lip to S-line |
0-2 mm |
1.5mm |
2mm |
2mm |
Treatment Results
Noticeable improvements were observed in the patient’s profile and lip positioning. Correction of anterior crossbite was obtained and Class I molar relationships were achieved bilaterally. Significant changes were observed in the maxillomandibular relationship as evidenced by the ANB and Wits appraisal (1˚, 3mm). The patient was satisfied with the treatment results.([Figure 4], [Figure 5])
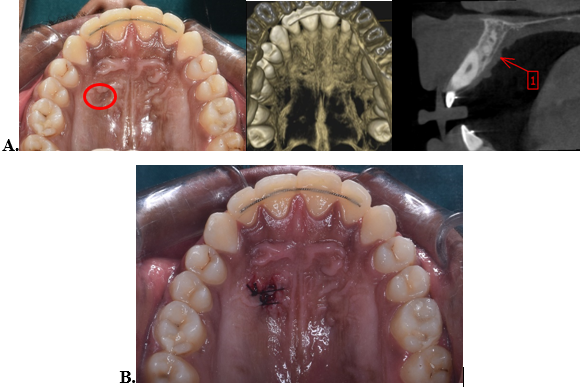
After six months, follow up was done, and the patient complained of unevenness of the soft tissues in the palatal implant site. A CBCT was advised for further investigation. The results of the investigation showed no abnormal skeletal findings. Soft tissue scarring was reported in the implant site. The patient was referred for periodontal therapy, and was advised for scar excision procedure to help promote proper healing of the implant site.
Also, during the investigation, an abnormal finding of localised periapical lesion near Canalis Sinuosus in the anterior maxilla was observed, which was diagnosed as idiopathic osteosclerosis. No intervention was planned.([Figure 6])
Discussion
Treatment success in developing Class III malocclusion, is determined by the individual’s growth and the timing of therapeutic intervention. Studies have proven the effectiveness of RME, along with face mask, in the treatment of growing Class III malocclusion patients.[2], [10] Now, it has been established as a standard protocol for the management of Class III malocclusion. Early intervention, such as during the primary dentition or the prepubertal growth period, has been advised.[11] Prepubertal treatment with RME and face mask protraction, in particular, results in favourable correction in the growth of maxilla and mandible. Here, in this case, the patient was already in permanent dentition when treatment started. Also, due to Covid-19, treatment had to be halted for quite some time. So, the decision to continue with the face mask therapy with rapid maxillary expansion, or wait for growth completion, was difficult. However, studies, evaluating the effect of age on the treatment response of face mask therapy with RME, have showed significant forward movement of maxilla with similar skeletal and dental effects in both young and older children.[12], [13] So, it was decided to continue the treatment and we were able to achieve favourable antero-posterior changes in the patient’s profile.
Orthopaedic forces for the protraction of maxilla are usually applied using tooth borne appliances. An undesirable effect of this approach is the mesial migration of the maxillary teeth, constriction of the maxillary canine space, along with periodontal defects as a result of the distribution of the force through the dental anchor units.[14] Application of orthopaedic stresses directly to the bone may be effective in overcoming these disadvantages. However, pure bone borne appliances are more invasive, and there is a risk of infection. The hybrid hyrax appliance introduced by Wilmes[15] provides an alternative for protraction of the maxilla with both bone and dental anchorage, where the undesirable effects of face mask with conventional tooth borne anchorage is mitigated. Significant advancement of the maxilla along with significant improvement in the mandibular sagittal position could be achieved. Also, the surgical invasiveness required is lower than that for purely bone borne appliances. In this patient, a significant skeletal improvement was achieved in the sagittal position of the maxilla, confirmed by the angle ANB (1°) and Wits (3mm). These values demonstrate that a greater advancement could be achieved with skeletal anchorage as compared with tooth borne anchorage.
Also, Alt-RAMEC protocol has shown improved results for maxillary protraction. Expansion and constriction of the maxilla in alternation, as used in Alt-RAMEC protocol, can enhance the protraction of the maxilla and offer a good result in children with more maturation of the sutures.[16], [17]
Mini-implants are frequently utilised in routine orthodontic treatment to improve the efficiency of orthopaedic or dental appliances. Mini-screws can have adverse effects and issues that might happen during their insertion, use, or removal. One such reported complication is disturbed wound healing or soft tissue scarring.[18] The palate is reportedly a safe zone with regard to scar formation. However, distinguishable scar like appearance of the tissue can frequently be observed after mini-screw removal.[19] Similarly, in our case, disturbed wound healing was reported with respect to the right palatal implant site. To address it and promote proper wound healing, surgical excision of the scar tissue was done.
Idiopathic osteosclerosis (IO), also called focal periapical osteopetrosis, is an intra bony, asymptomatic, benign, radiopaque lesion with unknown aetiology. The origin of IO may be associated as reaction to inflammation, occlusal trauma that might occur in tooth transition phase. IO usually develops early in life, and little changes occur after the affected individual is mature.[5] Normally, there is no requirement of any treatment. Some studies regarding orthodontic treatment and idiopathic osteosclerosis have reported delayed tooth movement in these areas,[20] while, a study conducted by Wang et al.[5] reported no obvious relation between idiopathic osteosclerosis and orthodontic treatment. In this case, the condition was diagnosed after treatment was completed and was benign with no symptoms, hence, no intervention was needed.
This case combined the benefits of face mask therapy and hybrid hyrax palatal implant anchorage with activation by Alt-RAMEC protocol for achieving maxillary protraction in an adolescent male patient.
Conclusion
Success in the orthopaedic treatment of growing Class III patients is determined by the individual’s growth and the timing of therapeutic intervention. However, there is always a risk that unpredictable growth of the mandible later on could indicate the need for potential orthognathic surgery during adulthood. Hence, proper case selection with a prolonged treatment time and long-term follow up is essential for a successful orthopaedic treatment of growing patients with Class III malocclusion.
Source of Funding
None.
Conflict of Interest
None.
References
- Hardy D, Cubas Y, Orellana M. Prevalence of angle Class III malocclusion: a systematic review and meta-analysis. Open J Epidemiol. 2012;2(4):75-82. [Google Scholar]
- Mcnamara J. An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1987;21(9):598-608. [Google Scholar]
- Liou E, Tsai W. A new protocol for maxillary protraction in cleft patients: repetitive weekly protocol of alternate rapid maxillary expansions and constrictions. Cleft Palate Craniofac J. 2005;42(2):121-8. [Google Scholar]
- Yilmaz B, Kucukkeles N. Skeletal, soft tissue, and airway changes following the alternate maxillary expansions and constrictions protocol. Angle Orthod. 2014;84(5):868-77. [Google Scholar]
- Wang S, Xu L, Cai C, Liu Z, Zhang L, Wang C. Longitudinal investigation of idiopathic osteosclerosis lesions of the jaws in a group of Chinese orthodontically-treated patients using digital panoramic radiography. J Dent Sci. 2022;17(1):113-21. [Google Scholar]
- Wilmes B, Ngan P, Liou E, Franchi L, Drescher D. Early class III facemask treatment with the hybrid hyrax and Alt-RAMEC protocol. J Clin Orthod. 2014;48(2):84-93. [Google Scholar]
- EL. Revista Dental Press De Ortodontia E Ortopedia Facial. . 2009. [Google Scholar]
- Park J, Emamy M, Lee S. Adult skeletal Class III correction with camouflage orthodontic treatment. Am J Orthod Dentofac Orthop. 2019;156(6):858-69. [Google Scholar]
- Yepes E, Quintero P, Rueda Z, Pedroza A. Optimal force for maxillary protraction facemask therapy in the early treatment of class III malocclusion. Eur J Orthod. 2014;36(5):586-94. [Google Scholar]
- Ngan P. Early timely treatment of Class III malocclusion. Semin Orthod. 2005;11(3):140-5. [Google Scholar]
- Campbell P. The dilemma of Class III treatment. Early or late?. Angle Orthod. 1983;53(3):175-91. [Google Scholar]
- Yüksel S, Uçem T, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23(5):559-68. [Google Scholar]
- Yavuz I, Halicioğlu K, Ceylan I. Face mask therapy effects in two skeletal maturation groups of female subjects with skeletal Class III malocclusions. Angle Orthod. 2009;79(5):842-50. [Google Scholar]
- Ngan P, Yiu C, Hu A, Hagg U, Wei S, Gunel E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur J Orthod. 1998;20(3):237-54. [Google Scholar]
- Wilmes B, Nienkemper M, Drescher D. Application and effectiveness of a miniimplant- and tooth-borne rapid palatal expansion device: the hybrid hyrax. World J Orthod. 2010;11(4):323-30. [Google Scholar]
- Liou E. Effective maxillary orthopedic protraction for growing Class III patients: A clinical application simulates distraction osteogenesis. Prog Orthod. 2005;6(2):154-71. [Google Scholar]
- Almuzian M, Mcconnell E, Darendeliler M, Alharbi F, Mohammed H. The effectiveness of alternating rapid maxillary expansion and constriction combined with maxillary protraction in the treatment of patients with a Class III malocclusion: A systematic review and meta-analysis. J Orthod. 2018;45(4):250-9. [Google Scholar]
- Giudice A, Rustico L, Longo M, Oteri G, Papadopoulos M, Nucera R. Complications reported with the use of orthodontic miniscrews: A systematic review. Korean J Orthod. 2021;51(3):199-216. [Google Scholar]
- Jung S, Choi Y, Lee D, Kim K, Chung C. Cross-sectional evaluation of the prevalence and factors associated with soft tissue scarring after the removal of miniscrews. Angle Orthod. 2015;85(3):420-6. [Google Scholar]
- Consolaro A, Consolaro R. Advancements in the knowledge of induced tooth movement: Idiopathic osteosclerosis, cortical bone and orthodontic movement. Dental Press J Orthod. 2012;17(4):12-8. [Google Scholar]
How to Cite This Article
Vancouver
Nongthombam H, Kumar M, Goyal M, Kumar S, Yadav E. Idiopathic osteosclerosis in a Class III patient treated with facemask therapy and hybrid hyrax- A case report [Internet]. J Contemp Orthod. 2023 [cited 2025 Oct 26];7(1):47-55. Available from: https://doi.org/10.18231/j.jco.2023.009
APA
Nongthombam, H., Kumar, M., Goyal, M., Kumar, S., Yadav, E. (2023). Idiopathic osteosclerosis in a Class III patient treated with facemask therapy and hybrid hyrax- A case report. J Contemp Orthod, 7(1), 47-55. https://doi.org/10.18231/j.jco.2023.009
MLA
Nongthombam, Haripriya, Kumar, Mukesh, Goyal, Manish, Kumar, Sumit, Yadav, Ekta. "Idiopathic osteosclerosis in a Class III patient treated with facemask therapy and hybrid hyrax- A case report." J Contemp Orthod, vol. 7, no. 1, 2023, pp. 47-55. https://doi.org/10.18231/j.jco.2023.009
Chicago
Nongthombam, H., Kumar, M., Goyal, M., Kumar, S., Yadav, E.. "Idiopathic osteosclerosis in a Class III patient treated with facemask therapy and hybrid hyrax- A case report." J Contemp Orthod 7, no. 1 (2023): 47-55. https://doi.org/10.18231/j.jco.2023.009
