Introduction
Class II, div I malocclusion exhibits a worldwide prevalence of 14% among children aged 12 to 14 years and is the most commonly observed malocclusion type in India. Clinical manifestations of class II, div I malocclusion include a range of severity in the skeletal base, with a predominantly class II molar relationship according to Angles classification. Additionally, it is characterized by class II canine and incisor relationships, maxillary incisors that are inclined forward, an increased overjet, and typically presents a convex facial profile accompanied by lips that are unable to fully close.1
In the management of class II div I malocclusion, various treatment approaches are commonly utilized. These include the application of a myofunctional appliance in individuals with ongoing facial growth, the strategic extraction of permanent teeth to facilitate dental camouflage and conceal the skeletal discrepancy, or the consideration of orthognathic surgery for patients who have ceased growing. When addressing class II malocclusions in individuals who are no longer experiencing growth, the extraction options may involve the removal of two maxillary premolars or two maxillary premolars along with two mandibular premolars in order to achieve correction. In growing patients, the extraction of four premolars is primarily recommended in cases of crowding in the mandibular arch, the presence of a cephalometric discrepancy, or a combination of both.2, 3, 4
The functional appliances used in growing patients are either removable or fixed in nature. Fixed devices, in contrast to removable appliances, generally do not rely on the patient's active participation and can be worn concurrently with multibracket therapy. This enables the correction of Class II malocclusion through a single-phase treatment approach.5 Functional appliances exert pressure on the mandible, causing it to move forward. This stimulates adaptive growth in the mandibular condyle and remodeling of the glenoid fossa. As a result, there is a notable increase in the effective length of the mandible and a correction of facial convexity.6
In this case report, we describe the treatment of a 14-year-old female patient who presented with a class II skeletal base resulting from a retruded mandible and a protruded maxilla, along with dentoalveolar protrusion. The treatment approach involved extractions followed by the implementation of forsus fatigue resistant device therapy. The Forsus fatigue-resistant device is composed of several components, including a universal spring module, an "L" pin, and a push rod. The push rod comes in five different sizes to accommodate various needs. These components are assembled in such a way that the push rod, of the appropriate size, connects directly to the lower archwire distal to the mandibular canines. The spring, on the other hand, attaches to the headgear tube on the maxillary first molar through the use of the "L" pin. 7 The main functions of the FRD appliance are limiting sagittal maxillary growth, promoting mandibular growth, inducing mesial movement of the mandibular arch, and distal movement of the maxillary arch. 8 However, one major side effect of FRD as with any functional appliances is undesirable forward tooth movement of the lower incisors. The proclination of the lower incisors hinders maximum skeletal correction. 9
Diagnosis
A 14 years old female patient reported to the department of orthodontics and dentofacial orthopedics, Government dental college and research institute, Bangalore with the chief complaint of forwardly places upper front teeth.
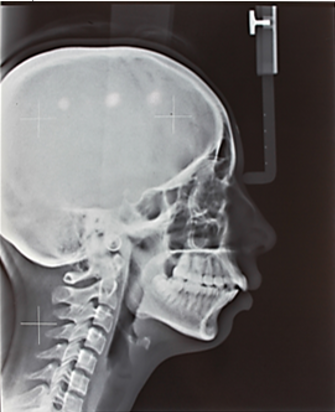
An extraoral examination revealed a mesocephalic head and mesoporsopic facial form. The patient’s profile was convex with posterior divergence, competent lips, acute nasolabial angle, and negative lip step. Reduced length of the mandible, reduced chin projection and low clinical FMA was also noted. No gross facial asymmetry was noted.(Figure 1)
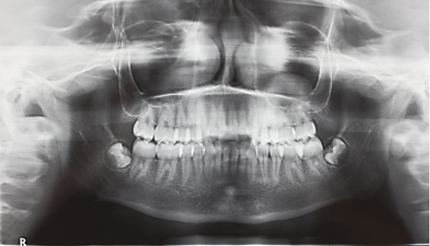
Her intraoral examination revealed, class 1 molar relation on the right side and end on molar relation on the left side, U-shaped upper and lower arches, proclined upper and lower anteriors with an overjet of 4mm, other individual dental irregularities such as crowding wrt 11,21, 31,41 and posterior crossbite wrt 36, were noted.(Figure 2)
Smile analysis revealed consonant smile arc with increased buccal corridor space.
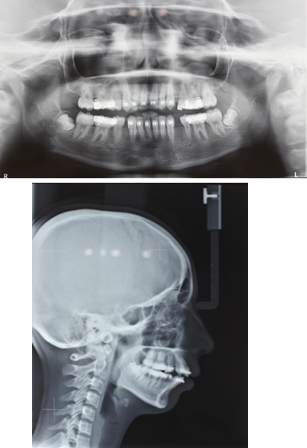
Cephalometric analysis revealed orthognathic maxilla and retrognathic mandible (Table 1 and (Figure 3).
Table 1
Cephalometric values
An orthopantomogram showed partially erupted mandibular third molars and congenitally missing maxillary third molars. There was no evidence of caries, restorations, or any other pathologies. (Figure 4)
Treatment Objectives
The main goals of orthodontic treatment in this case were to address molar relationships, minimize protrusion of the maxillary and mandibular dentoalveolar regions, achieve optimal overjet and overbite, establish a functional occlusion, reduce buccal corridor widths, and enhance facial and smile aesthetics.
Treatment alternatives
A removable functional appliance therapy was not an appropriate treatment choice, the option to correct the underlying anteroposterior dental and skeletal discrepancy by extraction of four first premolar teeth followed by Forsus fixed functional appliance therapy was accepted by the patient.
Extractions of first premolars were chosen instead of second premolars to correct the dentoalveolar protrusion in upper and lower arches.
Treatment progress
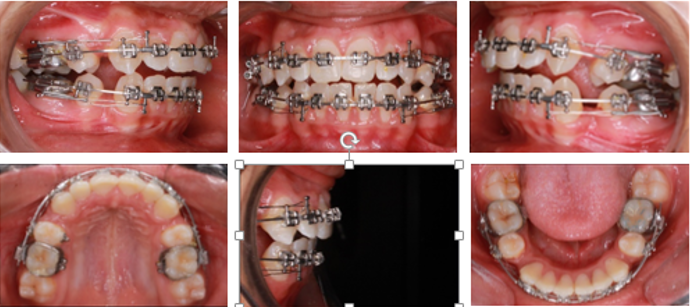
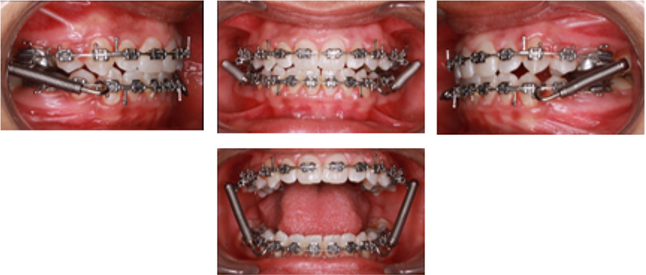
Extraction of 14, 24, 34, and 44, were carried out following which 0.022'' slot MBT brackets were bonded onto all the teeth, leveling and alignment of both arches were carried out using 0.016” NITI archwires, and the following sequence of archwires were used- 0.018 SS, 17*25 NITI, 19*25 SS. En masse space closure of upper and lower anterior segments was carried out using active tiebacks on continuous 19*25SS archwires. (Figure 5, Figure 6, Figure 7)
Extraction spaces were closed after six months, following which Forsus fixed functional appliance therapy was initiated (Figure 8).
The appliance was maintained for 7 months after which final finishing and detailing were carried out .0.014 NITI archwires were paced for 2 months for occlusal settling. Debonding was carried out after occlusal settling was completed and the retention phase was initiated with upper Begg’s wrap-around retainer with an anterior inclined plane and lower fixed lingual retainer.
Treatment Results
Noticeable enhancements were observed in both facial esthetics and occlusion. The treatment goals were successfully attained, as evidenced by the post-treatment evaluation of the patient's external facial features. The convexity of the profile reduced, buccal corridors diminished, and there was a remarkable improvement in smile aesthetics. (Figure 9)
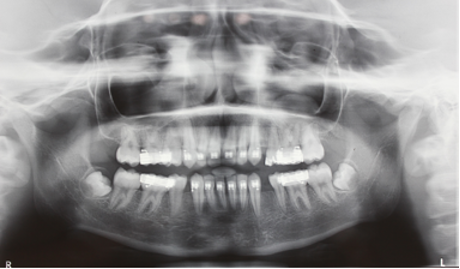
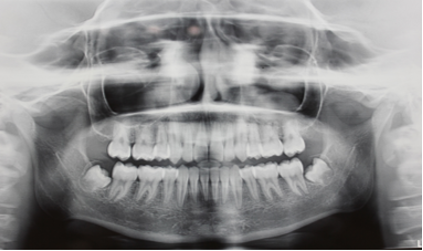
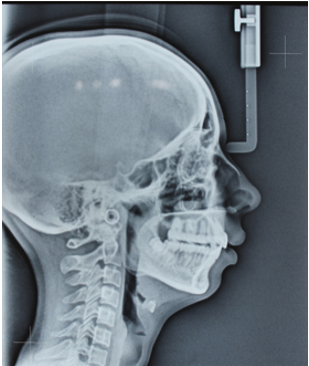
The post-treatment intraoral assessment revealed bilateral Class I molar and canine relationships, along with satisfactory intercuspation of the anterior and posterior teeth. (Figure 10). The panoramic radiograph showed satisfactory root angulation for all teeth. (Figure 11)
Following the functional appliance phase and completion of orthodontic treatment, the cephalometric analysis revealed minimal alterations in the skeletal components. However, notable labial inclination of both maxillary and mandibular incisors was observed in the dentoalveolar aspect. The clinical changes observed were verified through cephalometric superimpositions. (Table 1)
Discussion
Careful considerations towards facial esthetics, occlusion, and underlying skeletal discrepancy are essential to successfully treat class II malocclusion.
For the correction of dentoalveolar protrusion and moderate to severe crowding, extraction of permanent teeth will be required.
To treat the underlying skeletal discrepancy functional growth modification can be performed in growing patients and in adults surgical correction will be necessary.
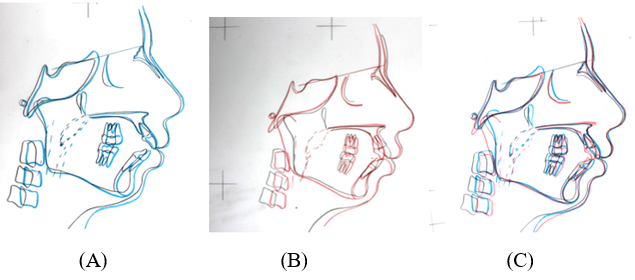
Figure 13
Superimposition of pre-treatment (black), mid- treatment (blue) (a) post-treatment (red) (b), comparison of pre, mid and post treatment cephalometric landmarks (c).
In children near the end of adolescence, a certain amount of skeletal changes can still be achieved by the use of fixed functional appliance. 10
In this particular case, the presence of proclined upper and lower anterior teeth, combined with a class II skeletal base caused by a retruded mandible, posed limitations to the advancement of the mandible through functional appliance therapy. As a result, the extraction of four first premolars was performed in order to address the proclination of the teeth and facilitate the desired advancement of the mandible.
The Forsus Fatigue Resistant Device (FFRD) is categorized as a fixed, hybrid functional appliance. It differs from rigid, fixed functional devices like the Herbst appliance due to its semi-rigid telescopic system, which provides flexibility in mandibular positioning. As a noncompliance device, the FFRD remains fixed in the patient's mouth, eliminating the need for the orthodontist to rely on the patient's cooperation. 11
The FFRD tends to push the upper molars distally and the lower molars mesially to correct the sagittal relationship while maintaining the vertical dimension. 12
Multiple studies have shown that FFRD corrected the sagittal discrepancy mainly by dentoalveolar changes when used for 5-6 months. 13
The cephalometric analysis revealed a reduction in ANB angle by 4º.
The lower incisor inclination was reduced by 11º after space closure, but increased by 3º after FFRD therapy. Thus, a total reduction in the lower incisor inclination by 8º. This increase in lower incisor inclination can be attributed to the tendency of the FFRD to procline the lower incisors.
The extraction treatment improved the incisor inclination which allowed the desired amount of forward positioning of the mandible without hindrance.
Extraction before fixed functional appliance therapy eliminated the natural dental compensations and provided stable dental relationships on the skeletal bases. It also counteracted the adverse effects of the fixed functional appliance on dental inclinations.
Therefore, extraction treatment along with the application of FFRD showed favorable dental skeletal and esthetic results.
To further improve the chin prominence in this patient, an anterior sliding genioplasty was advised. But, the patient is satisfied with the current results and is unwilling to undergo surgery. The one year follow-up photographs (Figure 14) reveals well maintained oral hygiene, stable functional occlusion .No further improvement in chin projection due to soft tissue growth was noted.
Conclusion
To effectively address the class II malocclusion caused by a retrognathic mandible and bidental protrusion, the FFRD was employed alongside the extraction of first premolars. The premolar extractions created sufficient space for achieving proper tooth inclination and eliminated any obstructions to mandibular advancement. In summary, a growing patient presenting a skeletal Class II malocclusion with a retruded mandible and prominently proclined dentition experienced successful treatment through a combination of a fixed functional appliance and premolar extractions