- Visibility 55 Views
- Downloads 5 Downloads
- DOI 10.18231/j.jco.2023.056
-
CrossMark
- Citation
Extraction of four premolars in hyperdivergent individuals, does it help? -A case report
- Author Details:
-
Ravindra Manerikar
-
Nandlal Toshniwal
-
Sumeet Mishra
-
Deeksha Devadiga
-
Shweta Nair *
Introduction
Although premolar extraction has long been recognized as a useful orthodontic treatment option, there is debate over how premolar extraction affects the vertical dimension. First, temporomandibular joint (TMJ) problems are thought to have premolar extraction as one of its etiologic factors by many.
Reduction in vertical dimension following extraction of maxillary and mandibular premolars has been reported to result from orthodontic forward migration of the posterior teeth. After that, the mandible is permitted to overclose, which is why it was believed that TMJ issues would probably arise. This notion is not supported by any published results.[1], [2], [3]
Another notion that has been put forth states that the extraction of first premolars causes the anterior teeth, especially the maxillary anteriors, to retract excessively. It is believed that this excessive retraction of the anterior teeth causes the mandible and condyles to shift posteriorly.[4], [5] It has long been known that TMJ issues are linked to posterior condylar dislocation. Similar to the preceding theory, no research study has supported this notion.
Garlington[6] attempted to reduce the vertical dimension through early removal of the remaining deciduous teeth and enucleation of the second premolars; although there was a statistically significant decrease in lower facial height, the MPA decreased by only 0.8°. Pearson[7] showed a mean decrease in MPA of 3.9° after premolar extraction, with vertical chin-cups used before and during orthodontic therapy. There was, however, no follow-up study to determine whether the mandibular plane angle reopened to its original position after treatment. Cusimano et al.[8] analysed the premolar extraction cases and found no over collapse of the vertical dimension; on the contrary, the vertical dimension was either maintained or slightly opened.
The present case describes orthodontic treatment in a patient with Class I malocclusion with increased maxillary anterior proclination with crowding in the mandibular arch and lower dental midline deviation, treated with four premolar extractions.
Case Report
Pre-treatment assessment
Patient details
The subject was a 19-year-old female, she came for treatment because she was concerned about the proclination and crowding of her upper anterior teeth with dental midline deviation and lower arch crowding. The patient had no other medical history.
Clinical examination
The skeletal assessment showed class 1 skeletal pattern with convex facial profile. Vertically, increased lower anterior face height proportions were noted. Acceptable facial symmetry and balance were observed on frontal examination. On soft tissue assessment, while lower lip was protrusive and they were potentially competent at rest ([Figure 1]).
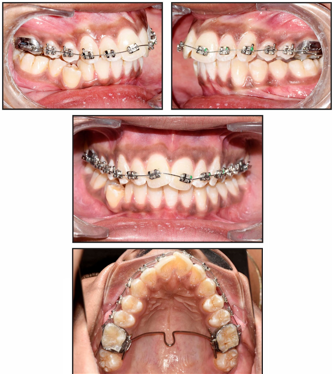
Intraoral examination showed that the patient was well motivated and demonstrated fair oral hygiene with good gingival health. Hyperpigmentation of gingiva was evident. All the teeth up to second molars were present in each quadrant ([Figure 2]).
Maxillary arch was presented with an ovoid arch form. It showed moderate labial segment crowding with proclined central incisors. Mandibular arch followed a U-shape with a buccally displaced right first premolar and increased proclination of the anterior teeth.
There was an overjet of 8 mm and increased overbite of 4mm. Buccal segments were in class 1 relationship on left side while Class 1 molar relationship with end-on canine relation was seen on the right side. The upper midline coincided with facial midline. The lower midline was shifted to right by 1.5 mm.








|
Parameter |
Pre-treatment |
Post-treatment |
|
Sagittal Skeletal Relationship |
|
|
|
SNA |
83° |
81° |
|
79° |
78° |
|
|
ANB |
4° |
3° |
|
Wits Appraisal |
3.4mm |
0.7mm |
|
Dental Base Relationship |
||
|
U1-NA |
35°, 9mm |
27°, 4mm |
|
L1-NB |
34°, 8mm |
24°, 4mm |
|
U1-Pal |
59° |
65° |
|
IMPA |
102° |
90° |
|
Dental Relationship |
||
|
Interincisal angle |
106° |
126° |
|
L1-APog |
5mm |
3mm |
|
Overjet |
8mm |
1.5mm |
|
Overbite |
4mm |
2 mm |
|
Vertical Skeletal Relationship |
||
|
FMA |
31° |
32° |
|
Maxillary-mandibular plane angle |
23° |
22° |
|
Lower anterior face height |
61mm |
60mm |
|
Total facial height |
133mm |
133mm |
|
Jarabak ratio |
67% |
63% |
|
U1-Palatal plane |
28mm |
26mm |
|
U6-Palatal plane |
21mm |
20mm |
|
L1-Mandibularplane |
39mm |
36mm |
|
L6-Mandibular plane |
27mm |
26mm |
|
Soft Tissues |
||
|
Lower lip to Ricketts E-line |
3mm |
1.5mm |
|
Nasolabial angle |
100° |
113° |
Relevant Radiographic Findings
There were no anomalies in the tooth forms or the surrounding structures, and the full set of permanent teeth was present. The third molars, upper and lower, were still growing. The bone level was typical.
Skeletal
The cephalometric analysis ([Table 1]) revealed a Class I Skeletal anteroposterior relationship with an ANB value of 4°, which supported the clinical findings. The vertical proportions assessed by FMA maxillo-mandibular plane angle, and face-height ratio were on the higher side of the normal range showing a vertical growth pattern and supporting the clinical findings.
Dental
Upper and lower incisors were proclined. As a result, the interincisal angle was reduced to 106°. Lower incisal edge was positioned anteriorly relative to point A-Pog line (+5 mm), consistent with lower anterior proclination.
Diagnostic Summary
The patient, a 19-year-old female, presented with the chief complaint of mal-aligned and forwardly placed upper and lower front teeth. On examination and analysis of relevant records, she was diagnosed with Angle's class I malocclusion on class I skeletal base with a vertical growth pattern. This was accompanied by an 8 mm overjet with proclination and mild crowding of upper and lower arches. She also presented an increased overbite and a midline discrepancy of 1.5 mm. Lips were protruded and incompetent at rest with decreased nasolabial angle.
Problem list
Bimaxillary proclination
Upper and lower labial segments crowding
Incompetent and protrusive lips
8 mm overjet
Reduced overbite
1.5 mm midline discrepancy
Aims and Objectives of Treatment
Relief of crowding
Level, align, and coordinate the dental arches
Reduce the overjet and achieve competent lips at rest
Correct the overbite
Correct midline discrepancy
Maintain class 1 molar relationship and achieve class 1 canine relationship on right side
Retain corrected results
Treatment plan
Treatment plan of extraction of all first premolars for crowding unravelling was decided. Upper and lower preadjusted edgewise fixed appliances (0.022 x 0.028" slot) with MBT - McLaughlin Bennett and Trevisi prescription was used.
To maintain anchorage during space closure as well as to have vertical control, a low-lying transpalatal arch was given.
Proposed retention strategy: Removable upper and lower wraparound retainers along with fixed boned retainers in the upper and lower arches
Prognosis for stability: provided that the general arch was maintained good occlusal interdigitation was achieved, the long-term stability of the treatment changes was considered good. In order to maximize the stability of overjet correction, it was important to retract the upper incisors within the control of the lower lip. However, owing to the large contact point displacements in the maxillary and mandibular labial segment, upper and lower bonded retainers along with removable wraparound retainers were considered appropriate.
Treatment Progress is depicted in [Figure 3], [Figure 4], [Figure 5], [Figure 6].
Post-treatment Assessment ([Figure 8], [Figure 9])
Occlusal features
After treatment, the incisor relationship was class I with an overjet of 1.5 mm and normal overbite ([Figure 7], [Figure 8]). The maxillary and mandibular midlines coincided with each other and the facial midline. The buccal segment relationship was maintained in a class 1 relationship bilaterally. No individual tooth movement was noticed after the treatment. Mutually protected occlusion was achieved with the orthodontic treatment.
Interpretation of Cephalometric Changes
Skeletal
The SNA and SNB values were reduced by 1° suggesting posterior remodelling of A and B points, respectively, because of upper and lower anterior retraction ([Table 1]).
A 3 mm increase in the whole anterior face height indicated that vertical development persisted throughout the course of the treatment. The vertical proportions, however, did not change significantly.
Dental
The upper incisor to SN plane angle was reduced by 8° (from 35° to 27°) following the retraction of the upper anterior. The lower incisor to mandibular plane was reduced by 10° (from 34° to 24°) following retraction of lower anteriors. There is slight decrease in the vertical dimension of the dental component seen in the linear measurements of incisors and molars to the palatal and mandibular planes.
Superimposition revealed that the upper and lower molars migrated very little in an anteroposterior direction. The lower incisal edge moved back by 3mm (5mm to 2mm) relative to A-Pog line.
Soft tissues
Nasolabial angle increased by 13° (from 100° to 113°). Lower lip position relative to Ricketts E plane was reduced by 1.5 mm. The shift in the positions of the upper and lower incisors during orthodontic treatment can account for both.
Critical appraisal
The patient was successfully treated by orthodontic treatment over 21 months.
The original treatment aims were accomplished, and the patient's presenting complaint was addressed and she was notably pleased with the treatment outcome. A good occlusal and aesthetic result was achieved.
Skeletal
There was no alteration in the skeletal link between the upper and lower jaws, but posterior repositioning of A and B points was observed with upper and lower incisor retraction, respectively.
The vertical relationship between the upper and lower jaw did not significantly change during the course of treatment, despite the continuation of vertical skeletal growth.
Dental
The 8mm overjet was successfully reduced within normal limits. The overbite was also increased to normal limits. The final occlusal fit was good.
The marginal gingival contour was irregular with the upper left central incisor, for which gingival recontouring was advised. But the patient did not agree to the same.
Soft tissues
The favourable soft tissue drape facilitated orthodontic treatment without detriment to dentofacial appearance. Lips were competent at the end of treatment, with the upper incisors under the control of the lower lip. These are favourable features for long-term stability of overjet correction. However, owing to the extent of the pretreatment contact point displacements in the maxillary and mandibular anterior teeth, upper and lower bonded retainers along with removable wraparound retainers were placed.
Iatrogenic sequelae
The post treatment radiographs identified no change in root and lower anteriors. There was a certain extent of decalcification evident on removal of the fixed appliances.
Discussion
In orthodontics, controlling vertical dimension has always been crucial. An essential feature of the human face, the vertical dimension frequently influences treatment plans. For instance, while treating patients who are hyper divergent, doctors may use techniques that are deemed intrusive, like tooth extractions or high-pull headgear, in an effort to reduce or at least not enhance the vertical dimension of the face. Patients with a short lower anterior face height experience the opposite.
Therefore, taking into account the vertical dimension, one of the most important treatment planning decisions that has also attracted a lot of attention in the literature is whether or not to extract teeth. This is an extremely controversial subject because some research suggests that evacuation of the posterior teeth can better manage the vertical dimension in hyperdivergent patients or lessen it altogether.[9], [10], [11]
The main rationale behind the supposition that tooth extractions reduce the vertical dimension is based on the wedge-effect concept, according to which the mesial movement of the molars during closure of the extraction spaces reduces the vertical dimension by anterior rotation of the mandible.[12] However, this concept has not been proven.
A possible explanation for this, as reported by Gkantidis et al.[13] is that the direction of the mesialization of the posterior teeth during space closure is parallel to the occlusal plane, and not to the maxillary and mandibular planes for the maxillary and mandibular teeth, respectively, as the wedge-effect theory suggests. The craniofacial complex, including the masticatory system, is complicated and should not be perceived as a simple articulator. There are probably more important factors than tooth numbers responsible for the establishment of the vertical positions of the teeth and the associated skeletal patterns, such as neuromuscular balance and function.
In this case, the delivery of low lying transpalatal arch not only helped in holding the molars in position but also prevented the worsening in the vertical dimension. Although the changes in measurements were not significant enough, but slight decrease in the linear values in the vertical dimension was noted.
Conclusion
This case report illustrates how a case with crowding and proclined anteriors can be managed with extraction of 4 premolars along with efficient conservation of anchorage at the same time. While there was no significant change in the vertical dimension, the planned goals set in the pre-treatment plan were successfully attained. Good intercuspation of the teeth was achieved. Treatment of the proclined and forwardly placed upper and lower anterior resulted in decrease in soft tissue procumbency and facial convexity. Patient had an improved smile and profile. The patient was very satisfied with the result of the treatment with a significant improvement in the patient aesthetics and self-esteem.
Source of Funding
The author received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- WJ Tulley. The role of extractions in orthodontic treatment. Br Dent J 1959. [Google Scholar]
- WE Wyatt. Preventing adverse effects on the temporomandibular joint through orthodontic treatment. Am J Orthod Dentofac Orthop 1987. [Google Scholar]
- GR Bowbeer. The sixth key to facial beauty and TMJ health. Funct Orthod 1987. [Google Scholar]
- JW Witzig, TJ Spahl. . The clinical management of basic maxillofacial orthopedic appliances 1987. [Google Scholar]
- WB Farrar, WL McCarty. . A clinical outline of temporomandibular joint diagnosis and treatment 1983. [Google Scholar]
- MA Garlington. Changes in mandibular plane angles after second bicuspid enucleation [master’s thesis]. Long Beach: University of Southern California. 1987. [Google Scholar]
- LE Pearson. Vertical control through use of mandibular intrusive forces. Angle Orthod 1973. [Google Scholar]
- C Cusimano, RP Mclaughlin, JH Zernik. Effects of first bicuspid extraction on facial height in high-angle cases. J Clin Orthod 1993. [Google Scholar]
- FF Schudy. The control of vertical overbite in clinical orthodontics. Angle Orthod 1968. [Google Scholar]
- M Garlington, LR Logan. Vertical changes in high mandibular plane cases following enucleation of second premolars. Angle Orthod 1990. [Google Scholar]
- A Aras. Vertical changes following orthodontic extraction treatment in skeletal open bite subjects. Eur J Orthod 2002. [Google Scholar]
- HW Fields, WR Proffit, WL Nixon, C Phillips, E Stanek. Facial pattern differences in long-faced children and adults. Am J Orthod 1984. [Google Scholar]
- N Gkantidis, D J Halazonetis, E Alexandropoulos, N B Haralabakis. Treatment strategies for patients with hyperdivergent Class II Division 1 malocclusion: is vertical dimension affected?. Am J Orthod Dentofacial Orthop 2011. [Google Scholar]
