Introduction
Orthodontic movement can be quick or slow, depending on the physical characteristics of the applied force, the size and the biological response of the periodontal ligament. According to Vardimon, Oren and Ben-Bassat, “tooth movement leaves marks on the bone”. In vertical direction, during tooth extrusion, the changes in the underlying bone tissue may not follow tooth displacement, leading to an increase in clinical length of the tooth crown, which is some times undesirable. According to Handelman (1996), labial and lingual/palatal bone cortical plates at incisors' apexes may represent anatomical limits to orthodontic tooth movement. 1, 2, 3, 4, 5, 6 Before choosing a course of treatment that entails anteroposterior movement of the incisor inside the jaws, it was necessary to evaluate the central incisor predilection and its relationship to the surrounding alveolar bone. The orthodontic tooth movement is limited by the cortical surfaces of the alveolar bone, beyond which fenestration or dehiscence may transpire. The cortical labial bone may dehisce as a result of the protrusion and maxillary-incisor vestibularization. The palatal-bone plate is similarly affected by tooth retraction. The teeth can be put back in their proper positions to reverse this impact.
Using a variety of mechanics and archwires, Yodthong et al. (2013) investigated changes in alveolar bone thickness during maxillary incisor retraction. They found a favorable correlation between the incisors' increased labial and total alveolar bone thickness and the retraction pace, change in inclination, and extent of incursion. 6, 7, 8 An essential component in defining the limits of tooth movement in alveolar bone. Unwanted orthodontic side effects, including as external root resorption, gingival recession, bone dehiscence, and fenestration, are likely to happen when the root travels past the alveolus and makes contact with the cortical bone. Labiolingual incisor movement is restricted by the mandibular incisor alveolar bone since it is mostly a compact, thin bone. As a result, tooth movement needs to be done carefully.6, 7, 8, 9, 10, 11, 12
Thus aim of the present study is to identify anatomic relationship between central incisor roots and alveolar bone thickness in individuals with variable sagittal malocclusions.
Aim
To identify anatomic relationship between central incisor roots and alveolar bone thickness in individuals with Angles Class I and Class II malocclusions and to also correlate if any sexual dimorphism among samples.
Materials and Methods
100 young adult patients, aged 15 to 30, whose pre-treatment lateral cephalograms were chosen from the pool of patients who reported to the Department of Orthodontics and Dentofacial Orthopedics, participated in the current cephalometric study. Every subject has given their informed written consent. On subjects, no invasive procedures have been performed. There are no negative effects on the patients from any of the techniques utilized in the study. Therefore, the current investigation is ethically justified and compliant.
Inclusion criteria
Angle’s Class I molar relationship. Angle’s Class II molar relationship, erupted permanent teeth irrespective of third molars, high quality radiographs.
Table 2
Landmarks used in the study
Table 3
Planes used in the study
Table 4
Parameters used in the study
Exclusion criteria
Previous orthodontic treatment, Class III molar relationship, Any craniofacial abnormalities, previous orthognathic surgery.
The sample comprised of 100 pre-treatment lateral cephalograms divided into 2 groups on the basis of Angle’s system of classification as Group I which includes patients with Angles’s Class I molar relationship and Group II which includes patients with Angles’s Class II molar relationship with 50 subjects in each group (Table 1).
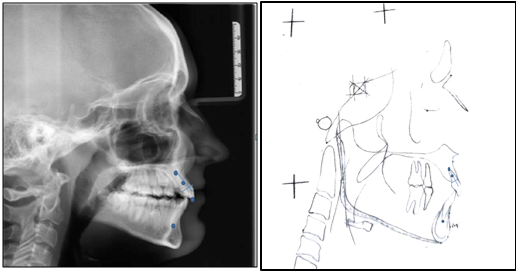
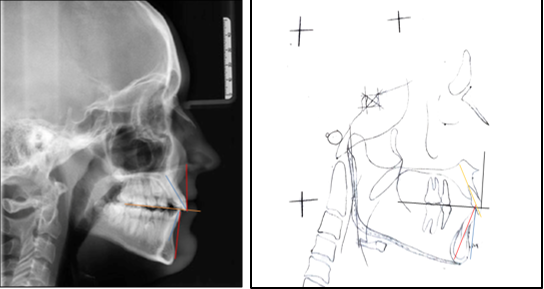
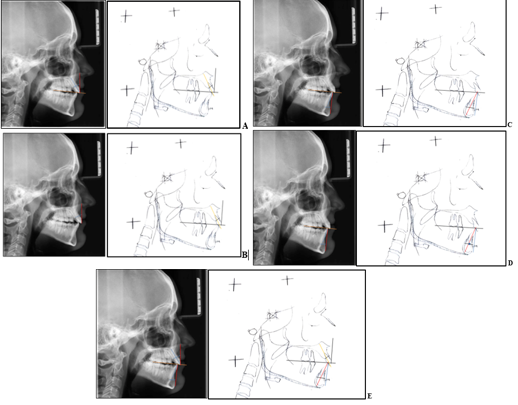
The same operator manually traced each lateral cephalogram in pencil on acetate paper. The upper arch, lower arch, first molars, inside and outside of cortical surfaces of the mandibular symphysis, and central incisors (left and right average) were among the structures tracked. The occlusal planes, incisal edges, root apices, incisor long axes, upper incisor cementoenamel junction (CEJ), and maxillary incisor root midpoint(Table 2, Figure 1), (Table 3 , Figure 2). Various parameters were then measured for both the groups (Table 4, Figure 3 a-e).
Statistical analysis
The statistical package for the social sciences (SPSS version 24.0 Inc., Chicago, IL, USA) was used to analyze all of the data. For every variable, the arithmetic mean and standard deviation were determined. In comparisons, a significance threshold of p <0.05 was applied. For a variety of criteria, the independent sample t-test was employed to identify potential statistically significant differences between the Class I and Class II. For the sample group (Class I and Class II), comparisons between males and females were also done using the independent samples t-test.
Results
When analysing the mean values of the variables, a comparison was made between Class I and Class II malocclusion. It was found that the U1-Lab score was statistically significantly higher in Class I individual compared to Class II patients (P=0.03). A significant increase in L1- ling values was also found in class II individual compared to class I (P=0.05). However, all other parameters were not significant between the groups (Table 5).
Table 5
Comparative analysis of maxillary mandibular alveolar bone thickness and inclination between class i and class II
The within-group comparison of Class I and Class II samples between males and females was found to be statistically significant with an increased value for mandibular alveolar bone thickness, as shown in Table 6 and Table 7. The Md-Alv thickness was significantly higher in males than in females (P=0.05) in both sample groups.
Table 6
Comparision between males and females in class I
Table 7
Comparison between males and females in class II
Discussion
The predisposition of the central incisors and their connection to the surrounding alveolar bone must be evaluated prior to any treatment decision involving AP movement of the incisor in the jaw. This study provided a unique opportunity to compare the thickness of the alveolar bone and the inclination of the incisor plane in different sagittal malocclusions.
When analysing the mean values of the variables, Class I and Class II malocclusion were compared. U1-pal was found to be statistically significant with an increased value for Class I patients. The root positions observed in Class I subjects were consistent, with the upper incisor root center points almost invariably occupying the anterior third of the alveolar process and the mandibular root tips located approximately in the center of the alveolus. In the Class II sample, a similar pattern prevailed for the maxillary incisors, but the root apices of the mandibular incisors were posterior to the center of the alveolus and their inclination was greater than in optimal occlusions, indicating the presence of dental compensations. Studies by Gracco et al.(2009), 11, Nahas-Scocate et al. (2014), 2 Tian et al. (2015). 13 Yamada et al. (2007), 14 Al-Abdwani et al. (2009) 15 came to similar conclusions and were in agreement with our study. The results of Hassan et al. (2015) 16 and Sun et al. (2021) 17 were not in agreement.
The change in the overall thickness of the alveolar bone at the apical level was related to the change in the inclination and extent of intrusion by the maxillary incisors. The change in alveolar bone height of the protruded permanent mandibular incisors may be influenced by the change in angulation between the mandibular plane and the axis of the mandibular central incisors. Studies by Gracco et al. (2009), 11 Nahas-Scocate et al. (2014), 2 Tian et al. (2015). 13 Yamada et al. (2007).14 Al-Abdwani et al(2009) 15 came to similar conclusions and were in agreement with our study. Hassan et al. (2015) 16 and Sun et al (2021) 17 disagreed (Table 5).
The thickness of the mandibular alveolar bone was statistically significant and higher in men than in women. All other variables were found to be non-significant. The greater values of alveolar bone thickness in men can be explained by a bony compensation phenomenon (remodelling). Cassetta et al. (2013). 18 Adiguzel et al. (2017). 19 Zhang et al. (2016), 20 Gakonyo et al. (2018). 21 Nahass et al. (2015). 22 Lee et al. (2019), 23 Sheerah et al.(2019). 24 Adiguzel et al. (2017) were in favour of our study and concluded that gender was significantly related to maxillary alveolar bone thickness. The authors Fuentes et al. (2015), 25 Ono et al. (2008), 26 Farnsworth et al. (2011), 27 Choi et al. (2009), 28 Park et al. (2008) 29 found that alveolar bone thickness does not vary by gender.
The extent of disruption and change in inclination should be accurately assessed when planning Orthodontic Treatment for cases requiring correction of the anterior teeth to avoid gummy smiles or camouflaged grins. More appropriate treatment options can be surgical intervention if there are risks of undesirable effects as a result of changes at alveolar bone thickness. The incidence of alveolar loss has been shown to be higher in people with osteoporosis or low bone mass, even though the link is not fully understood. A chronic deficiency of vitamin D and calcium, which leads to increased removal of calcium from bones, including the alveolar bone, is likely to cause a deficit in calcium balance. This loss of bone can weaken the periodontium. Resistance to bone resorption may be increased by the thickness of bones in buccal alveolar cortex. There is an increased risk of alveolar bone loss in patients with low bone mass or osteoporosis. This type of bone loss may accelerate the signs and symptoms of Periodontal Disease. Almost all social classes, including children and adolescents, are affected by the lack of vitamin D.
Limitation of present study
This study was conducted on a small population of the Solan region, so the results cannot be generalized to other African and European populations; More research is needed to extrapolate the results to other populations. Many individuals in the Class II sample had excessive overbite, suggesting that few natural dental compensations were present; a sample with a wider range of malocclusions might yield different findings. The present study was based solely on lateral cephalograms, which may have multiple dimensional errors. Therefore, modern diagnostic tools such as cone beam computed tomography could also have been included in the study.