Introduction
Class II malocclusion is one of the most common problem around the globe affecting about one third of the patients seeking orthodontic treatment. McNamara stated that a retrusive mandible is the most common feature of this malocclusion. 1 Functional appliances can be used to correct both skeletal and dental problems in these patients. These appliances have been used since the 1930s. despite their long history, there is still much controversy surrounding their use, mode of action, and effectiveness. Twin block appliance therapy is more effective at correcting class II malocclusion through skeletal changes than most other appliances, making it suitable for early orthodontic treatment in patients with class II malocclusion. 2 Myofunctional therapy is not a universal treatment approach for all growing patients, and several factors must be considered when choosing the best course of care. Saddle angle is one of the most crucial factors in the success of myofunctional treatment.
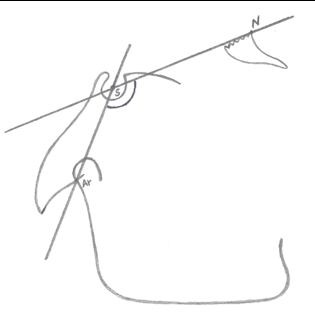
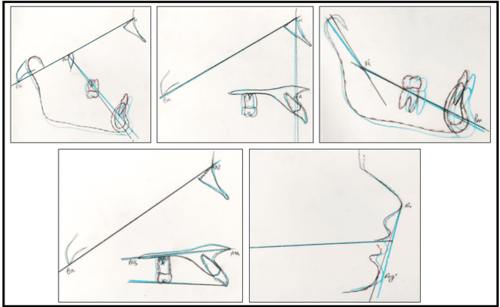
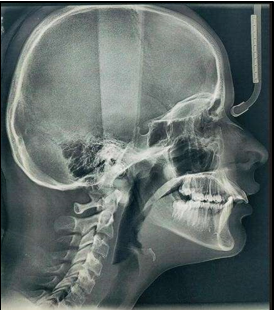
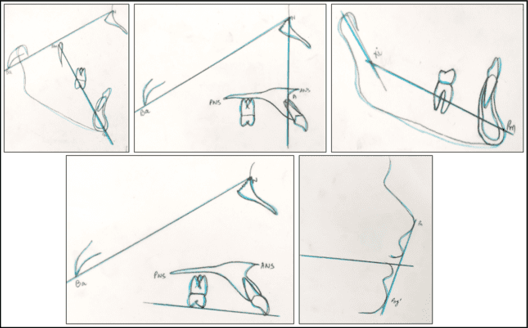
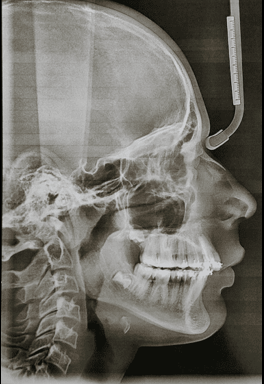
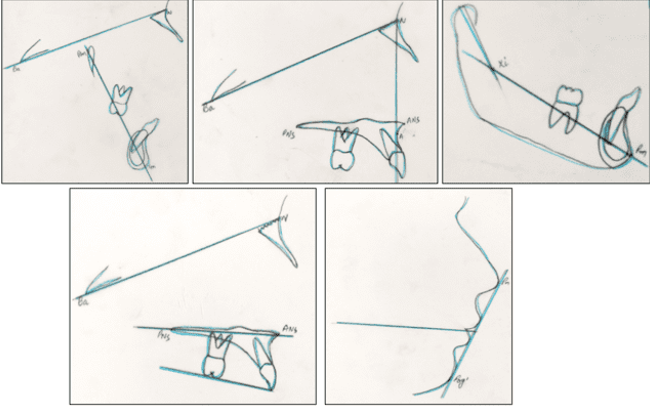
Saddle angle: Saddle angle, a concept introduced by Rakosi, is the angle between the anterior and posterior cranial bases.3 (N-S-Ar; nasion-sella- articulare) as shown in Figure 1.
A large saddle angle indicates a posterior position of the fossa and a small saddle angle indicates an anteriorly positioned fossa.
Graber, Rakosi, and Petrovic suggested that a large saddle angle often indicates a posteriorly displaced condyle and mandible relative to the cranial base and maxilla. This is unless the fossa position is compensated for specific angular (articular angle) and linear (ramal length) relationships. Notably, a non-compensated posterior mandibular position due to a large saddle angle is highly resistant to correction through functional appliance therapy. 4
There are three case reports in this study that describe growing patients treated with a twin block appliance to correct skeletal class II malocclusion. All parameters were favorable for myofunctional therapy, except for the increased saddle angle. These cases demonstrate the impact of saddle angle (N-S-Ar) on the effectiveness of myofunctional treatment.
Case Report 1
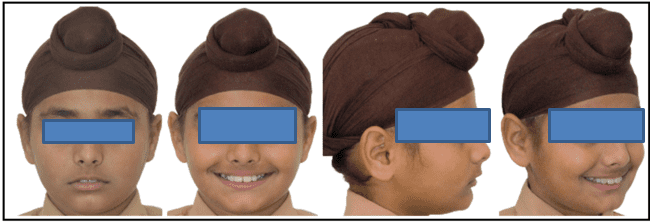
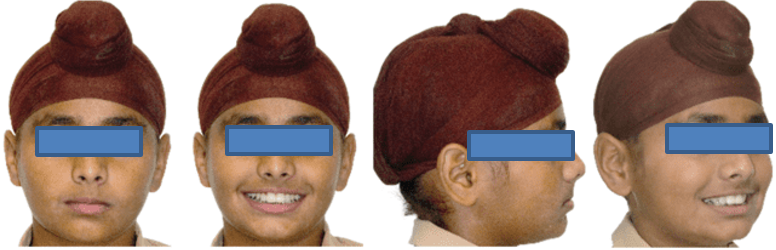
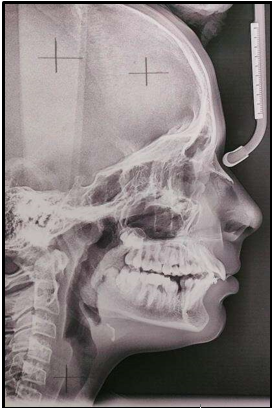
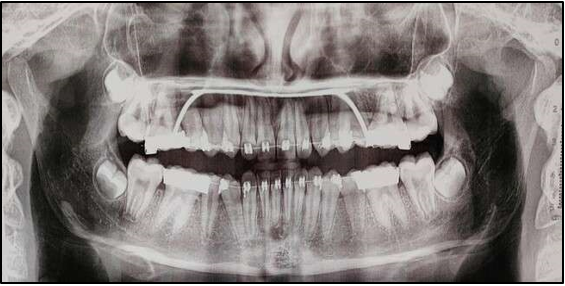
12 years old prepubertal male diagnosed with class II skeletal base, orthognathic maxilla, retrognathic mandible, straight path of closure. He had Angle’s class II malocclusion: increased inclination of maxillary anteriors and retroclined mandibular incisors, increased overjet and overbite, deep curve of the spee. The upper and lower midlines did not coincide. Patient’s profile was convex, with an obtuse nasolabial angle (Figure 1, Figure 2). The cephalometric measurements are mentioned in Table 1.
Growth prediction
(i) CVMI 2 (acceleration stage): 65 – 85% growth remaining (Figure 4)
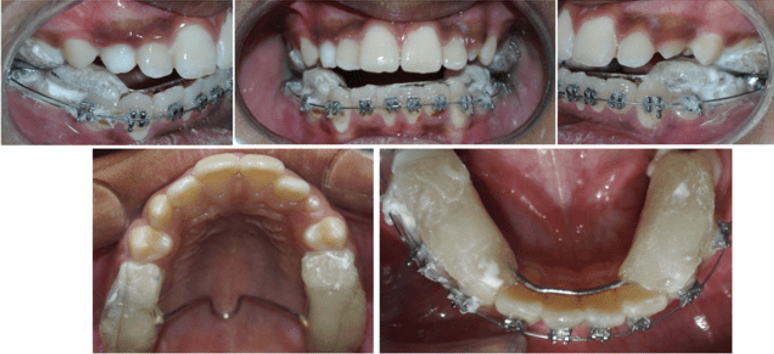
The treatment plan was divided into two phases:
Treatment outcome
After two months of completion of phase 2 (levelling and alignment), it was found out that the treatment had undergone relapse. (Figure 12, Figure 15)
Cranial base to point A angle was the same, cranial base to point B angle had decreased due to retropositioned mandible (ANB = 8⁰) resulted in increased overjet.
`
Table 1
Comprehensive cephalometric evaluation
Case Report 2
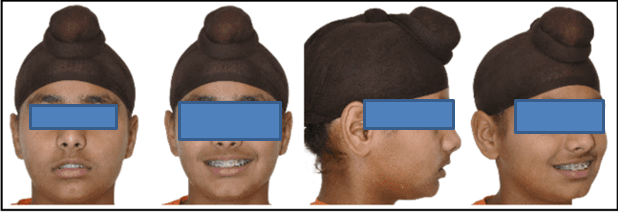
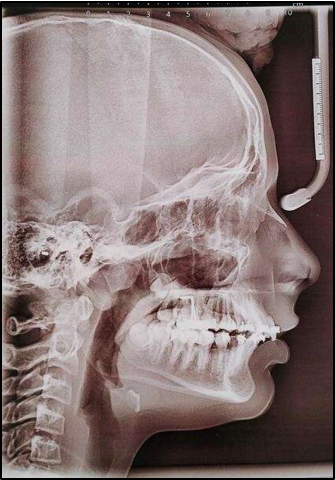
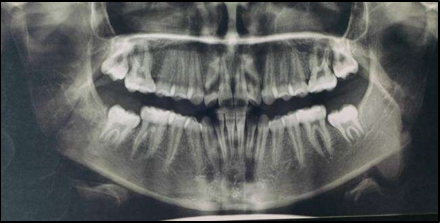
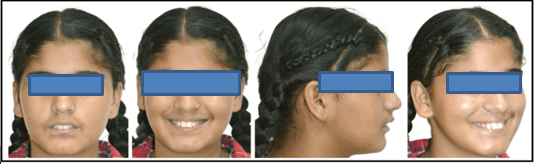
13 years old prepubertal female diagnosed with class II skeletal base, orthognathic maxilla, retrognathic mandible, straight path of closure with Angle’s class II malocclusion: increased inclination of maxillary anteriors and retroclined mandibular incisors, increased overjet and overbite. Patient’s profile was convex, with an obtuse nasolabial angle. (Figure 17) The cephalometric measurements are mentioned in Table 2.
Problem list
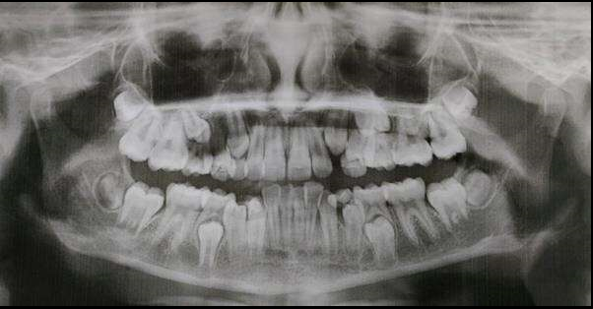
Dental problem (Figure 18)
Soft tissue problems
Table 2
Comprehensive cephalometric evaluation
Growth prediction
I. CVMI 3 (transition stage) represented 25 – 65% of remaining growth. (Figure 19)
Treatment plan
Considering the growth status of the patient the treatment plan decided for this patient was twin block therapy followed by fixed mechanotherapy.
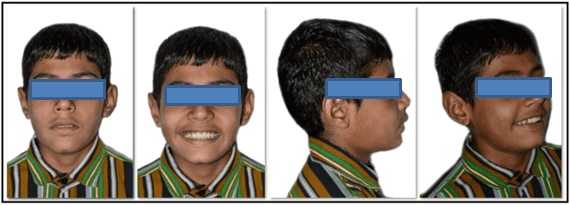
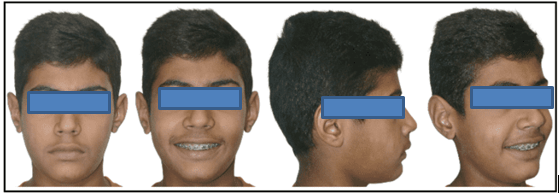
Case Report 3
12 years old prepubertal male diagnosed with class II skeletal base, orthognathic maxilla, retrognathic mandible, straight path of closure with Angle’s class II malocclusion: increased inclination of maxillary anteriors and proclined mandibular incisors, increased overjet. Patient’s profile was convex, with an obtuse nasolabial angle (due to upturned nose). (Figure 27) The cephalometric measurements are mentioned in Table 3.
Problem list
Dental problem (Figure 28)
Soft tissue problems
Convex profile
Obtuse nasolabial angle
Potentially incompetent lips
Retruded lower lip
Protrusive upper lip
Table 3
Comprehensive cephalometric evaluation
Treatment objectives
To achieve a Class I skeletal base
To achieve Class I molar and canine relations on both sides
To achieve normal overjet
To correct the inclination of the upper and lower anteriors
To close spacing in upper and lower arch
To achieve levelling and alignment
To achieve a harmonious soft tissue profile
Treatment plan
Considering the growth status of the patient the treatment plan decided for this patient was twin block therapy alongwith fixed mechanotherapy.
Discussion
Management of class II malocclusion has wide spectrum of options. Growth modulation is often the best option for growing patients. Functional appliances can be used to achieve this goal, and they can be very effective in producing the desired outcome.
The twin block functional appliance has several well-documented advantages over other functional appliances. It is better tolerated by patients, 5 more durable, easier to repair, and can be used in both permanent and mixed dentition. Additionally, patients can function normally while wearing the twin block, which makes it easier to wear full-time.
Dr. William J. Clark has stated that patients must be actively growing in order to achieve favorable skeletal changes during treatment. Treatment that coincides with the pubertal growth spurt may produce a more rapid skeletal response. 6
Baccetti et al. found that the best time to start Twin-block therapy for Class II malocclusion is during or slightly after the onset of the pubertal growth spurt.7
To achieve a successful outcome, it is important to choose the right treatment approach for each patient. Not every growing patient with a Class II skeletal base is a good candidate for functional appliance therapy. In addition to do the clinical examination, it is essential to perform a cephalometric evaluation to assess the patient's individual needs before deciding whether to use functional appliances.
Saddle angle emerges as a crucial cephalometric parameter that warrants careful consideration prior to embarking on myofunctional treatment.
Characterized by a sharp drop in early infancy, the saddle angle exhibits a subsequent slowdown in its descent, finally reaching a plateau a few years after puberty. This initial rapid decline, averaging around 5 degrees within the first two years, occurs irrespective of Class I or Class II occlusion. Notably, individual variations in the angle's progression become less pronounced as one matures, with a strong tendency towards stability post-puberty. 8
In a study done by Al Maaitah et al stated that, saddle angle was found to be larger in Class II skeletal relationship as compared to Class I and Class III skeletal relation. 9
Increased saddle angle is present in the cases with posteriorly positioned glenoid fossa and decreased saddle angle is present in cases with anteriorly positioned glenoid fossa. In orthognathic profiles, this deviation in the position of glenoid fossa is compensated by the length of ramus and if not, results in either prognathic or retrognathic profile. Cases with large saddle angle are difficult to treat with functional appliance. 4
In the present study, all the factors are in favour of myofunctional therapy except the saddle angle that was increased.
Following successful completion of the 9-month Phase 1 functional therapy, we achieved all our treatment goals in our first case. Notably, the twin block treatment led to an increase in mandibular unit length, subsequently reflected in a rise in the SNB angle, consistent with C.M. Mills' findings in his study. 10 However, after just 2 months of fixed mechanotherapy, relapse occurred. The remaining two cases exhibited no response to the initial myofunctional phase. In all three cases, an elevated saddle angle emerged as the culprit behind treatment relapse, indicating significant mandibular retropositioning relative to the cranial base prior to treatment initiation.
The effectiveness of myofunctional therapy is contingent upon a multitude of factors, rather than a single determinant. This study has demonstrated the substantial influence of saddle angle on achieving successful outcomes in myofunctional treatment.
Conclusion
Functional appliances are widely used in growing patients to achieve the best possible outcomes. However, it is important to remember that every patient is unique, and the effectiveness of treatment can vary depending on a number of factors, most notably the saddle angle.
The saddle angle is a critical determinant of success in functional appliance therapy. Saddle angles between 123° ± 5° are most conducive to successful treatment outcomes. Cases with large saddle angles are less likely to respond to treatment or may relapse.
Meticulous patient selection and personalized treatment planning are essential not only for achieving successful results in myofunctional treatment, but also prevents unnecessary discomfort to the patient and avoiding the wastage of their time on unnecessary treatments.