- Visibility 543 Views
- Downloads 79 Downloads
- Permissions
- DOI 10.18231/j.jco.2024.041
-
CrossMark
- Citation
To evaluate the cortical bone thickness for ideal placement of infrazygomatic crest (IZC) and mandibular buccal shelf (MCS) bone screws in patients with different facial pattern using cone-beam computed tomography (CBCT)
Abstract
Aims: This study aimed to measure the cortical bone thickness at different anatomical sites of InfraZygomatic Crest and Mandibular Buccal Shelf region for the ideal placement of IZC and MBS screws respectively in patients with different facial patterns using CBCT.
Materials and Methods: Total participants were divided into 3 groups- GROUP A: horizontal growth pattern (FMA <22°); GROUP B: average growth pattern (FMA 22°-28°); GROUP C: vertical growth pattern(FMA >28°). Sixty CBCT images were taken into consideration. They were converted into standard DICOM format. Bone thickness were measured in the InfraZygomatic Crest (IZC) of the maxilla and in the Mandibular Buccal Shelf (MBS) region of the mandible using the Kodak CareStream CS 9300 Software.
Results: The results indicate that there was a highly statistical significant difference seen in the overall cortical bone thickness of IZC and MBS at various anatomical sites. The highest mean thickness was found to be at the MB70◦ maxillary 1st molar and distal root of the mandibular 1st molar. There was no difference in the bone thickness at the IZC region and at the MBS region seen between the horizontal and vertical facial patterns whereas the average facial patterns show the highest mean thickness but was not statistically significant
Conclusions: The study conducted on the Indian population yielded results demonstrating the possibly appropriate position for the IZC bonescrews and MBS bonescrews suggested that placing the IZC bonescrews at the mesiobuccal root of the maxillary 1st molar at an angulation of 70◦ and the MBS bonescrews at the distal root of the mandibular 1st molar at 11mm from the cementoenamel junction irrespective of the facial patterns could provide positive results.
Introduction
The miniscrews placed in the extra-alveolar sites are called bonescrews that have been used frequently in orthodontic practice. Bone screws are placed far away from the roots i.e extra-radicular in order to provide optimal safety from damaging the roots and prevent premature loosening as well as the failure of the same also, they do not interfere with tooth movement.[1], [2]
Recently, extra-alveolar locations such as the InfraZygomatic Crest (IZC) and the Mandibular Buccal Shelf (MBS) have been utilized since they provide enough bone quality and density for miniscrew insertion and they located far from dental roots.[3] They can be used for canine retraction, en mass retraction, anterior retraction,intrusion of posterior teeth,and distalization of the maxillary and mandibular arch.[4]
Lin et al. stated that the infra zygomatic crest is located superiorly and laterally to the first and second molar areas. In adults, it is above the maxillary first molar, however in children, it is between the second premolar and first molar. The Mandibular Buccal Shelf, on the other hand, is found in the posterior region of the mandible on both sides. It is anterior to the oblique line of the mandibular ramus, and buccal to the roots of the first and second molars.[4], [5], [6]
Recently, researchers explored that the cortical bone thickness differs in patients with different facial types. [7] The facial morphology is a crucial factor in orthodontics as it influences the growth prediction, the anchorage, and mainly the goals of orthodontic treatment. [8] It is also important for the clinician placing bonescrews to be aware of any differences in cortical bone thickness between and within regions of the jaws. Thicker cortical bone has been reported for the mandible than the maxilla. There also appear to be differences in each jaw, with the thickest cortical bone in the molar region, followed by the premolar and incisor regions, respectively. [9] It has been noted that bone quality, as well as quantity, differs among different populations. [10]
Therefore, the aim of this study was to use CBCT imaging to assess the cortical bone thickness at different anatomical sites of the mandibular buccal shelf region and the infra-zygomatic crest region in order to determine the best location for MBS and IZC screws, respectively. Additionally, this study evaluated and compared the cortical bone thickness at these sites among people from the Indian population with different facial patterns.
Materials and Methods
After obtaining permission from the Institutional Ethics Committee, patients who required full mouth CBCT images as well as lateral cephalogram as a part of their treatment were taken into consideration. From the Out-Patient Department of Orthodontics and Dentofacial Orthopedics, a total of 60 patients, aged 18 to 25, who reported for orthodontic treatment were selected.
The inclusion criteria were as follows: 1. Participants between 18 to 25 years of age. 2. No history of orthodontic treatment. 3. No severe crowding. 4. Fully erupted permanent dentition. 5. Subjects who were indicated CBCT for their orthodontic treatment. The exclusion criteria were:1. Craniofacial anomalies. 2. Periodontal disease/ bony lesions. 3. Missing permanent maxillary and mandibular teeth. 4. Systemic diseases. 5. Impacted teeth except third molars.
Total 60 participants were divided into 3 groups based on Frankfort Mandibular Plane angle(a line tangent to the lower border of the mandible and the F-H plane) - GROUP A: Participants with horizontal growth pattern(FMA <22°); GROUP B: Participants with average growth pattern(FMA 22°-28°); GROUP C: Participants with vertical growth pattern(FMA >28°).
Sixty CBCT images were taken into consideration. They were converted into standard DICOM (Digital Imaging and Communications in Medicine) format. Using the Kodak Care Stream CS 9300 Software, bone thickness was assessed in the Mandibular Buccal Shelf (MBS) area of the mandible and the Infra Zygomatic Crest (IZC) of the maxilla.
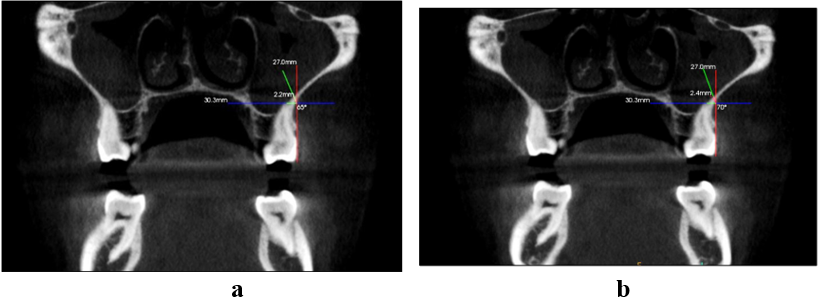
To assess the safe regions of bone screws implanted in the IZC region of the maxilla, nitially, on the coronal view, the images from the CBCT’s were oriented such that the occlusal plane was parallel to the lower border of the display window. Then, at the axial view the green line was passed through the molars root that was going to be assessed at that moment. Then, at the coronal view a blue line was passed through the tip of the same root. On the same view, a red line was placed tangent to the buccal cortical bone. The bone thickness was then measured at 65° and 70° [Fig.1(a), (b)] angles in the coronal plane at the site where the red and blue lines meet. These measurements were done over the mesio-buccal root of first molar, the distobuccal root of first molar and between the roots of the second molar.
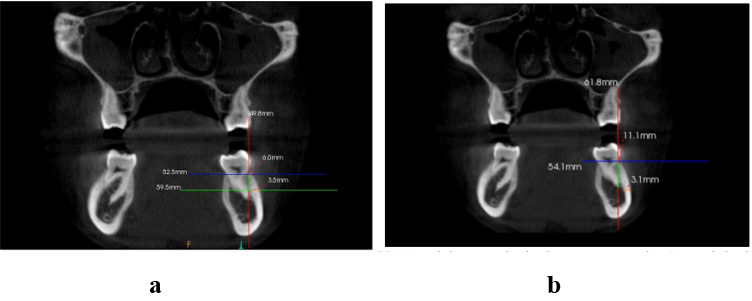
To assess the safe regions of bone screws implanted in the MBS region of the mandible the following procedure was done: Three multiplanar views were used as guidance: red line for the coronal plane, green line for the sagittal plane, and blue line for the axial plane. Initially, the axial plane was oriented so that the root furcations of the mandibular molars became collinear. The sagittal plane was then oriented so that the green line passed through the molar's root's long axis, which was to be evaluated at that particular moment. Finally, the coronal plane was reoriented according to the sagittal plane. The measurements were performed on the mesial and distal roots of the mandibular first and second molars. All roots were evaluated transversely and vertically. On the coronal plane, a blue line was passed through the CEJ. A vertical red line was drawn tangent to the root surface. Evaluation of the transverse buccal bone thickness was made apically at 6mm [Fig.2(a)] and 11 mm [Fig.2(b)] from the cementoenamel junction (CEJ) because extra-alveolar miniscrews are usually placed >10 mm apical to the CEJ.
Statistical data analysis
Data entries was done in Microsoft Office Excel 2010 and analyses of results was done using Statistical product and service solution (SPSS) version 22 software. Descriptive statistics such as mean and standard deviation was calculated for quantitative variables. The p value was fixed at 0.05. Data normality was checked using Shapiro Wilk test. One-way ANOVA f test was used to compare overall cortical bone measurements between different facial profiles and different locations. Tukeys post hoc test was used for pairwise comparison between groups.
Results
Our results show that overall cortical bone thickness of IZC across various anatomical sites varied in a way that was highly statistically significant. The highest mean thickness was found to be at the MB70◦ maxillary 1st molar. There was a highly statistical difference seen in the inter-group comparison between MB65◦ and PR65◦, MB65◦ and PR70◦, MB70◦ and DB65◦, MB70◦ and DB70◦, MB70◦ and PR65◦ , MB70◦ and PR70◦. There was a statistically significant difference seen between MB65◦ and DB65◦, DB70◦ and PR65◦.([Table 1], [Table 2])
The results show that overall cortical bone thickness of MBS across various anatomical sites varied in a way that was highly statistically significant. At the distal root of the mandibular first molar, the highest mean thickness was found. A highly statistically significant difference was seen in the inter-group comparison of the mandibular first and second molar distal roots. There was a statistically significant difference seen between mesial and distal roots of mandibular 1st molar, mesial and distal roots of mandibular 2nd molar. ([Table 3], [])
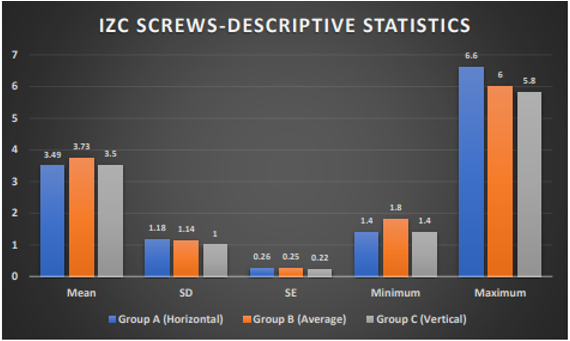
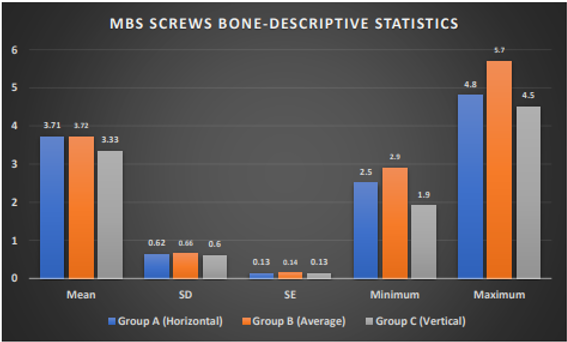
There was no difference in the bone thickness at the IZC region and at the MBS region seen between the horizontal and vertical facial patterns whereas the average facial patterns show the highest mean thickness but was not statistically significant.([Figure 3], [Figure 4]).
|
IZC(in mm) |
Mean |
SD |
SE |
Minimum |
Maximum |
|
MB 65° |
3.13 |
1.05 |
1.05 |
1 |
6.4 |
|
MB 70 ° |
3.53 |
1.1 |
1.1 |
1 |
6.6 |
|
DB 65° |
2.6 |
1.03 |
1.03 |
1 |
5.8 |
|
DB 70° |
2.73 |
1.04 |
1.04 |
1.2 |
6 |
|
PR 65° |
2.11 |
0.82 |
0.82 |
0 |
5.3 |
|
PR 70° |
2.32 |
0.87 |
0.87 |
0 |
5.5 |
|
Group |
Comparison |
P value |
|
MB 65* vs |
MB70* |
P=0.234 |
|
DB 65* |
P=0.041* |
|
|
DB 70* |
P=0.239 |
|
|
PR65* |
p≤0.001** |
|
|
PR70* |
p≤0.001** |
|
|
MB 70* vs |
DB65* |
p≤0.001** |
|
DB70* |
p≤0.001** |
|
|
PR65* |
p≤0.001** |
|
|
PR70* |
p≤0.001** |
|
|
MB 65* vs |
DB70* |
P=0.978 |
|
MBS (in mm) |
Mean |
SD |
SE |
Minimum |
Maximum |
|
Mandibular 1st Molar - Mesial |
2.96 |
0.71 |
0.09 |
1.4 |
4.7 |
|
Mandibular 1st Molar - Distal |
3.32 |
0.71 |
0.09 |
1.9 |
5.7 |
|
Mandibular 2nd Molar - Mesial |
3.11 |
0.67 |
0.08 |
1.3 |
4.8 |
|
Mandibular 2nd Molar – Distal |
2.75 |
0.56 |
0.07 |
0.9 |
3.9 |
|
Group |
Comparison Group |
P value, Significance |
|
Mandibular 1st Molar – Mesial Vs |
Mandibular 1st Molar – Distal |
p = 0.02* |
|
Mandibular 2nd Molar – Mesial |
p = 0.639 |
|
|
Mandibular 2nd Molar – Distal |
p = 0.286 |
|
|
Mandibular 1st Molar – Distal Vs |
Mandibular 2nd Molar – Mesial |
p = 0.306 |
|
Mandibular 2nd Molar – Distal |
p < 0.001** |
|
|
Mandibular 2nd Molar – Mesial vs |
Mandibular 2nd Molar - Distal |
p = 0.018* |
Discussion
Skeletal anchorage using TAD’s have been widely used by orthodontists in the recent years to provide absolute anchorage. However, a major disadvantage of these miniscrews is that they need to be repositioned frequently due to their proximity to the adjacent roots especially during distalization of the of the maxillary and mandibular dental arches as they interfere with the path of tooth movement. [1], [2], [3], [4], [5], [7], [11]
The extra-radicular sites are the best locations for placing miniscrews because they have thicker bone and are farthest from the roots. In the maxilla, it is the InfraZygomatic Crest (IZC) area whereas in the mandible, the Mandibular Buccal Shelf (MBS) area. The Temporary Anchorage Devices (TADs) used in these extra-alveolar sites are also known as bonescrews as they are deeply embedded in the bone and have increased length (10 to 12mm) and diameter (2mm). [11]
A number of studies have been carried out to assess the cortical bone thickness in the Mandibular Buccal Shelf area and the InfraZygomatic Crest separately, with the majority of these studies being carried out in the Caucasian population. There are a very few studies that have been conducted for both, the IZC and MBS region and further correlating them with the facial pattern. So our study was designed by incorporating all the above parameters.
The cortical bone thickness was measured at six different sites in the InfraZygomatic Crest region for our study. These sites included the maxillary first molar's mesiobuccal root at an angulation of 65◦ and 70◦ (MB65◦, MB70◦), the maxillary first molar's distobuccal root at an angulation of 65◦ and 70◦ (DB65◦, DB70◦ ), and the middle of the second molar at an angulation of 65◦ and 70◦ (PR65◦, PR70◦). Measurements were taken at four distinct sites in the Mandibular Buccal Shelf region,i.e. the mesial and distal root of the 1st molar, mesial and distal root of the 2nd molar at 6mm and 11mm each from the cemento-enamel junction. The insertion location of these extra-radicular bonescrews is typically more than 10mm from the cemento-enamel junction, hence we only took the measurements taken at 11mm into consideration.
The results of our study showed that there was highly statistically significant (p<0.001) difference between the different anatomical sites for the ideal placement of IZC bonescrews with higher values seen at the mesiobuccal root of the maxillary 1st molar at an angulation of 70◦ ([Table 1]).
These results disagreed with those of studies by Murugesan A et al. and Almir Lima et al., which discovered that, particularly in high-angle subjects, the IZC bone thickness was greater above the mesiobuccal root of the second maxillary molar than that of the first molar.a limitation of their study that a very small sample size was taken into consideration. [12], [13]
We also observed that the bone thickness in the IZC region decreased posteriorly. ([Table 1]) In the IZC region we found the following results: the highest bone thickness was found at MB70◦ the mean thickness was 3.53±1.1mm followed by MB65◦ , DB70◦ DB65◦ , PR70◦ and PR65◦ with a mean thickness of 3.13±1.05mm, 2.73±1.04mm, 2.6±1.03mm, 2.32±0.87mm and 2.11±0.82mm respectively. ([Table 1]).
We found an increase in the bone thickness with an increase in the insertion angulation ([Table 1]) which was similar to the findings of Eric J. W. Liou et al. They measured the thickness of the infrazygomatic crest at various angulations above the maxillary first molar in their studies. The postulated results were similar to our findings in which they stated that greater the miniscrew insertion angle, the thicker the bone at the IZ crest area would be. [14]
Numerous studies of similar types have also been conducted to determine the best location for the MBS bonescrews in the mandibular buccal shelf area. The various anatomical sites for the best placement of MBS bonescrews differed statistically significantly (p<0.001), according to the results we obtained. We found the highest mean thickness of 3.32±0.71mm in the distal root of the mandibular 1st molar whereas the lowest thickness was found in the distal root of the mandibular 2nd molar with a mean of 2.75±0.56mm. ([Table 3])
We also evaluated correlation of the horizontal, average and vertical facial types with the cortical bone thickness in the IZC and MBS region. However, the results of our study found that there was statistically no significant difference in the cortical bone thickness in the IZC ([Figure 3]) and MBS ([Figure 4]) region in the individuals with different facial types. The mean thickness found in the IZC region for horizontal growth pattern was 3.49±1.18mm whereas for the average and vertical growth pattern it was 3.73±1.14mm and 3.5±1.0mm respectively.
Patients with an increased vertical skeletal pattern have been discovered to have thinner cortical bones, which might compromise the mini-implants' primary stability. It is unclear, nevertheless, if the infrazygomatic area likewise exhibits this decreased cortical bone thickness. The angle of placement and direction of loading force in mini implants put in the IZC area are significant factors that may influence the failure rate. [10]
Within the constraints of this study, it is reasonable to assume that, in the case of India, the mesiobuccal root of the maxillary first molar at an angulation of 70◦ represents the most favourable overall anatomic location for the ideal positioning of the infrazygomatic crest bonescrew. This might be because the cortical bone thickness in this region is higher than in the posterior areas. As mentioned before, it's found that the IZC region's bone thickness reduces posteriorly. For the mandibular buccal shelf bonescrew placement the most favourable site is at the distobuccal root of the mandibular first molar. This site is also clinically accessible in most patients with a straight driver that facilitates placement. In patients with limited mouth opening, this site is easily accessible. If not, then a contra-angle insertion instrument should be selected for better access. However, with placement, it is important to consider the potential proximity to the inferior alveolar nerve and to keep in mind that CBCT should be taken into consideration for the same.
The IZC and MBS bonescrews can be placed at these mentioned anatomical sites, irrespective of the facial pattern of an individual.
One of the limitations of our study is that the sample size was comparatively smaller and it did not represent the patient with different growth pattern equally. Moreover, this study evaluated only Indian population, the bony characteristics of the IZC and MBS could be different in other ethnic groups. Further studies are necessary to evaluate IZC and MBS characteristics in different ethnic groups.
Conclusion
The study conducted on the Indian population yielded results demonstrating the possibly appropriate position for the IZC bonescrews and MBS bonescrews. Thus from the selected samples it is suggested that placing the IZC bonescrews at the mesiobuccal root of the maxillary 1st molar at an angulation of 70◦ and the MBS bonescrews at the distal root of the mandibular 1st molar at 11mm from the cementoenamel junction irrespective of the facial patterns could provide positive results.
There was no statistically significant difference seen in the overall cortical bone thickness for ideal placement of IZC and MBS bonescrews in patients with different facial patterns. Hence, we can state that there is no difference in bone thickness between the average, horizontal, and vertical facial types in IZC and MBS region.
Source of Funding
None.
Conflict of Interest
None.
References
- Ghosh A. Infra-zygomatic crest and buccal shelf-Orthodontic bone screws: A leap ahead of micro-implants-Clinical perspectives. J Indian Orthod Soc. 2018;52(4):127-68. [Google Scholar]
- Ozdemir F, Tozlu M, Cakan D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J orthod Dentofac Orthop. 2013;143(2):190-6. [Google Scholar]
- Liu H, Wu X, Tan J, Li X. Safe regions of miniscrew implantation for distalization of mandibular dentition with CBCT. . Prog Orthod. 2019;20:1-8. [Google Scholar]
- Pathak S, Patil T, Mahamuni A, Jaju K, Rai R. Mandibular buccal shelf and infra zygomatic crest-A safe zone for mini screw insertion. Indian J Orthod Dentofac Res. 2019;5(2):60-2. [Google Scholar]
- Nucera R, Giudice AL, Bellocchio A, Spinuzza P, Caprioglio A, Perillo L. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. . Angle Orthod. 2017;87(5):745-51. [Google Scholar]
- Lin J, Liou E, Yeh C. Intrusion of overerupted maxillary molars with miniscrew anchorage. J Clin Orthod. 2006;40(6). [Google Scholar]
- Sadek M, Sabet N, Hassan I. Three-dimensional mapping of cortical bone thickness in subjects with different vertical facial dimensions. Prog Orthod. 2016;17(1):1-7. [Google Scholar]
- Tsunori M, Mashita M, Kasai K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. . Angle Orthod. 1998;68:557-62. [Google Scholar]
- Farnsworth D, Rossouw P, Ceen R, Buschang P. Cortical bone thickness at common miniscrew implant placement sites. Am J Orthod Dentofac Orthop. 2011;139(4):495-503. [Google Scholar]
- Matias M, Flores-Mir C, Almeida MD, Silva D, Vieira B, Freitas KD. Miniscrew insertion sites of infrazygomatic crest and mandibular buccal shelf in different vertical craniofacial patterns: a cone-beam computed tomography study. Korean J Orthod. 2021;51(6). [Google Scholar]
- Shaikh A, Jamdar A, Galgali S, Patil S, Patel I, Sushilamma M. Efficacy of Infrazygomatic Crest Implants for Full-arch Distalization of Maxilla and Reduction of Gummy Smile in Class II Malocclusion. Dent Pract. 2021;22(10):1135-78. [Google Scholar]
- Murugesan A, Sivakumar A. Comparison of bone thickness in infrazygomatic crest area at various miniscrew insertion angles in Dravidian population-A cone beam computed tomography study. Int Orthod. 2020;18(1):105-19. [Google Scholar]
- Lima A, Domingos R, Ribeiro A, Neto J, Paiva JD. Safe sites for orthodontic miniscrew insertion in the infrazygomatic crest area in different facial types: A tomographic study. Am J Orthod Dentofac Orthop. 2022;161(1):37-45. [Google Scholar]
- Liou E, Chen P, Wang Y, Lin J. A computed tomographic image study on the thickness of the infrazygomatic crest of the maxilla and its clinical implications for miniscrew insertion. . Am J Orthod Dentofac Orthop. 2007;131(3):352-8. [Google Scholar]
How to Cite This Article
Vancouver
Ansari S, Nene S, Kalia A, Hegde A, Joshi J, Patil SR. To evaluate the cortical bone thickness for ideal placement of infrazygomatic crest (IZC) and mandibular buccal shelf (MCS) bone screws in patients with different facial pattern using cone-beam computed tomography (CBCT) [Internet]. J Contemp Orthod. 2024 [cited 2025 Oct 25];8(3):275-280. Available from: https://doi.org/10.18231/j.jco.2024.041
APA
Ansari, S., Nene, S., Kalia, A., Hegde, A., Joshi, J., Patil, S. R. (2024). To evaluate the cortical bone thickness for ideal placement of infrazygomatic crest (IZC) and mandibular buccal shelf (MCS) bone screws in patients with different facial pattern using cone-beam computed tomography (CBCT). J Contemp Orthod, 8(3), 275-280. https://doi.org/10.18231/j.jco.2024.041
MLA
Ansari, Saba, Nene, Salil, Kalia, Ajit, Hegde, Ashwith, Joshi, Juhi, Patil, Sagar Rajesh. "To evaluate the cortical bone thickness for ideal placement of infrazygomatic crest (IZC) and mandibular buccal shelf (MCS) bone screws in patients with different facial pattern using cone-beam computed tomography (CBCT)." J Contemp Orthod, vol. 8, no. 3, 2024, pp. 275-280. https://doi.org/10.18231/j.jco.2024.041
Chicago
Ansari, S., Nene, S., Kalia, A., Hegde, A., Joshi, J., Patil, S. R.. "To evaluate the cortical bone thickness for ideal placement of infrazygomatic crest (IZC) and mandibular buccal shelf (MCS) bone screws in patients with different facial pattern using cone-beam computed tomography (CBCT)." J Contemp Orthod 8, no. 3 (2024): 275-280. https://doi.org/10.18231/j.jco.2024.041
