Introduction
Cleft lip and palate (CLP) is the most common congenital deformity, with greater frequency among Asians compared to other ethnic groups having aetiologic variability, with relative contributions from hereditary and environmental factors. 1, 2 The World Health Organisation (WHO) reported that CLP affects around 1 in 1000 – 1500 newborns globally its Global Oral Health Status Report 2022. 3 This condition can arise between the fourth and twelve weeks of gestation due to a lack of fusion between the medial nasal and maxillary processes of the primary palate or the palatal units of the secondary palate, 4 and is known to modify the features of the midface and anterior maxillary area, which can range from minor to severe alterations. 5 Ultrasonographers, including obstetrician-gynaecologists and radiologists, doing standard 20-week ultrasound screening may detect these abnormalities prenatally. 6
In the past, early detection of cleft palate was less common; however, over the years, several novel techniques have been developed, such as 3D transabdominal ultrasound, prenatal magnetic resonance imaging (MRI), amniocentesis, and the "equal sign," which has led to an increase in the antenatal diagnosis of facial clefts. 7, 8 There are various benefits to detecting orofacial clefts antenatally, including less anxiety before labor and preparedness for the birth of a child with a cleft, and it makes it possible to discuss treatment alternatives before delivery. 9 On the other hand, elective termination of pregnancy (ETOP) may also result from advancements in the prenatal detection of cleft lip or palate. 10
A multidisciplinary team approach is very much necessary to prevent induced pregnancy termination for cleft patients, who have an excellent prognosis and require optimal treatment. 11 It includes early diagnosis, monitoring facial growth and dental eruption, determining surgical timing, correcting soft tissue and skeletal abnormalities, and ensuring proper positioning of craniofacial structures. 12 The success of this team approach, which includes ultrasonographers, medical and dental specialists including orthodontists, 13 relies on the broad general knowledge possessed by each team member.14 Therefore, the purpose of this study was to assess the knowledge, awareness, and attitudes of obstetrician-gynecologists, and radiologists regarding current treatment regimens for CLP and their perspectives on elective termination of pregnancy for the same cause.
Materials and Methods
A cross-sectional questionnaire survey was conducted on obstetrician-gynecologists and radiologists in the form of a Google Form via social network with a short description of the study, and the responses were collected over 6 months. The Institutional Ethics Committee (IEC) at Sri Rajiv Gandhi College of Dental Science & Hospital Bangalore, approved the study (IEC No. SRGCDS/2023/237). The questionnaire included 19 questions in 2 parts. Part 1 focused on demographic information (Table 1), and Part 2 on knowledge, awareness, and attitude towards CLP and their views on termination of pregnancy for the same cause.
Of the total 120 participants, 68 were gynecologists and 52 were radiologists, of which eighty-four (70.00%) were females and thirty-six (30.00%) were males. Out of which six (5.00%) specialists had an experience of more than 10 years, Thirty (25.00%) of them with 4-8 years, fifty (41.70%) of them with 2-4 years, and thirty-four (28.30%) of them with < / = 2 years of experience respectively. Fifty-one (42.50%) of the specialists worked in medical colleges & hospitals, forty-one (34.20%) of them in private hospitals, seventeen (14.20%) of them in private practice, and eleven (9.20%) of them in public hospitals (Table 1).
The specialists were enquired about the likelihood of a prenatal diagnosis of CLP using ultrasound, the number of abortions resulting from CLP, whether they have encountered CLP-related abortions, whether they have advised parents about available treatment options for CLP, their knowledge of CLP, and the preoperative care of newborns with CLP.
Statistical analysis
Statistical analysis of the data obtained was performed using SPSS software (SPSS for Windows version 20.0; SPSS Inc, Chicago, IL, USA). Descriptive statistics were generated for the assessed parameters. Categorical variables were analyzed using percentages. Data was analyzed with, Pearson chi-square tests, and multivariable generalized estimating equations. Spearman Rank correlation was used to assess construct validity. Statistical significance was set to P <.05.
Table 1
Sociodemographic characteristics
Results
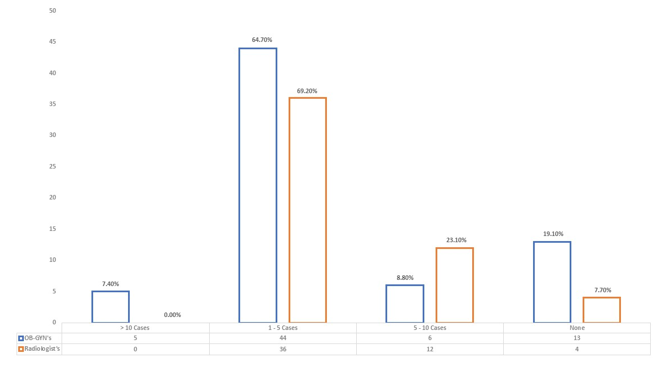
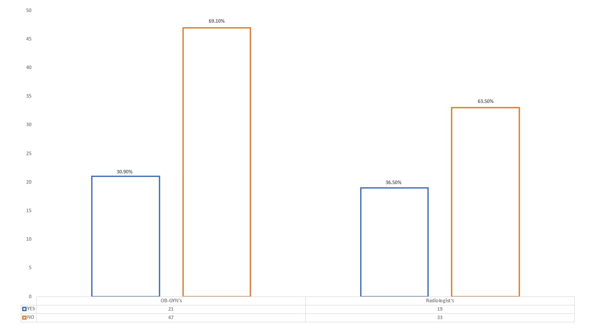
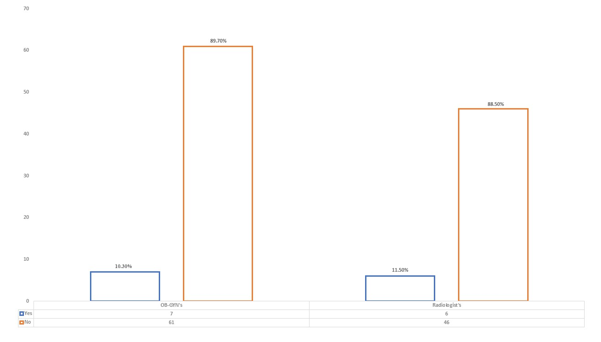
68 gynecologists and 52 radiologists responded to the survey (Table 1). The study showed a statistically significant variation in the number of cases identified by each specialty about 89% of gynecologists and 92.3% of radiologists can identify CLP during the initial assessment of the fetus using ultrasound technique (Figure 1), whereas 30.90% of gynecologists and 36.50% of radiologists have encountered elective termination of pregnancy due to CLP (Figure 2), and 89.70% of gynecologists and 88.50% of radiologists do not know pre-surgical orthopedic procedures for CLP (Figure 3).
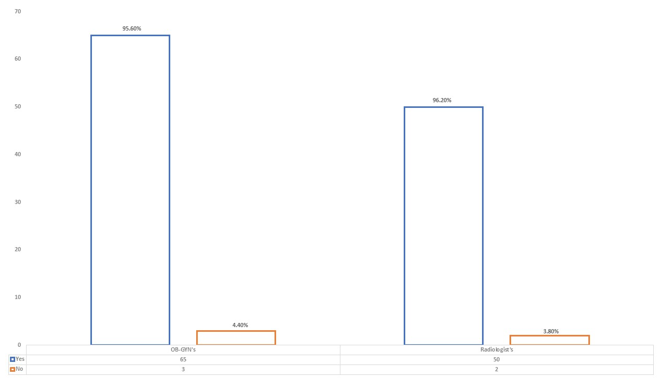
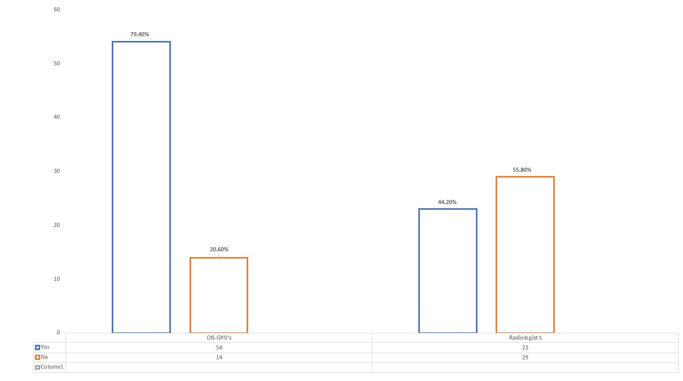
Even though 95.60% of gynecologists and 96.20% of radiologists claimed a high detection rate of CLP through ultrasonography (Figure 4), only 79.40% of gynecologists and 44.20% of radiologists preferred providing first information to parents after the diagnosis of CLP was confirmed using ultrasonography (Figure 5).
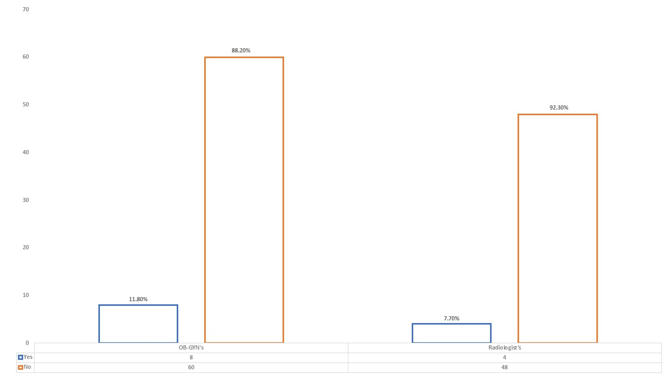
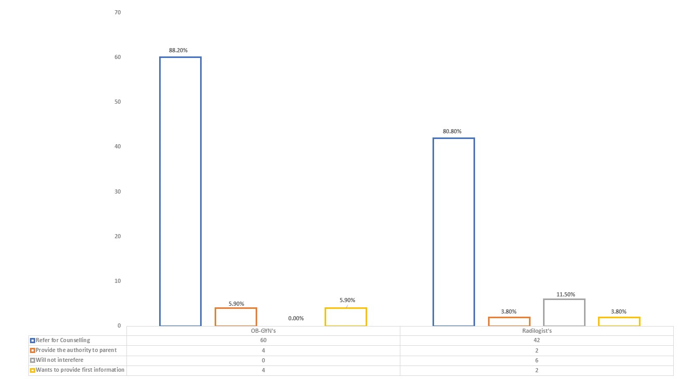
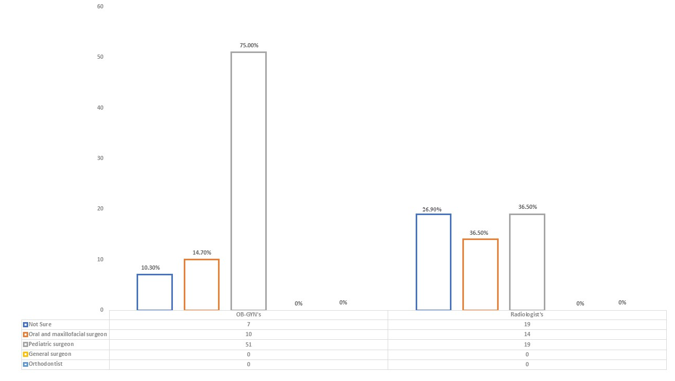
As 88.20% of gynecologists and 92.30% of radiologists’ knowledge of the NAM/LATHAM procedure was minimal (Figure 6), 88.20% of gynecologists and 80.80% of radiologists (Figure 7) preferred referring the potential parents for proper counseling regarding the anomaly. Still there existed an ambivalent opinion among specialists on where to refer the patient for the same (Figure 8).
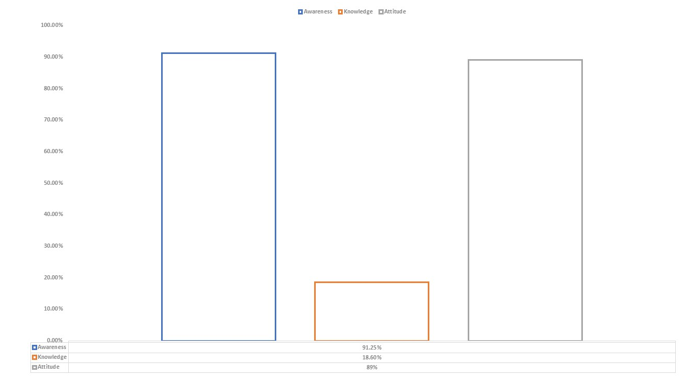
On average, the specialists had sufficient awareness regarding the anomaly of 91.25% with their knowledge of pre-surgical orthopedic procedures being minimal at 18.60%. They exhibited a positive attitude of 89% towards having more knowledge about the same for their further practice (Figure 9), with no statistically significant difference existing in the knowledge level about CLP and its treatment regimens among both groups (P value >.05).
Discussion
CLP is still considered to be a controversial topic in the field of medical and healthcare sectors concerning diagnosis and management due to its distinct facial characteristics when compared to non-cleft patients. 15 Early identification of these facial anomalies that occur in the late first or early second trimester of pregnancy, is very much necessary to have a better prognosis and treatment outcome. In this regard prenatal ultrasonography has become the standard of care, increasing the prenatal diagnosis of anomalies like oral clefts. 16 However prenatal detection of oral clefts is a topic of debate in terms of parental, social, and ethical implications, 17 which also provides numerous benefits for parents, including psychological preparation for the abnormality, information on feeding issues, and effective management of the condition. 18
Concerns have also been raised regarding the rising rate of pregnancy terminations in cases of fetuses prenatally diagnosed with isolated non-syndromic clefts. 19 Non-syndromic oral clefts are nonlethal birth defects with an excellent functional and aesthetic prognosis; furthermore, they present moral dilemmas surrounding the termination of pregnancy. 20, 21
The prevalence of pregnancy terminations due to a solitary facial cleft alone varies from 0 to 92%. 22 A study on the effect of prenatal diagnosis on the occurrence of oral clefts by Bronshtein et al., 20 throughout 10 years, including 24,000 scans, 15 cases of cleft lip were identified, out of which 14 were terminated, 19 In contrast, a follow-up study stated that out of 30,000 prenatal ultrasound scans, 24 cases with cleft lips were identified, 23 of which were terminated.
Another study by Berkowitz et al., 23 concluded that it is a true tragedy that abortions cannot be stopped in these situations.
The present survey involved, a total of 68 obstetricians and 52 radiologists of which 21 obstetricians and 19 radiologists, have faced various cases of elective termination of pregnancy in fetuses who were diagnosed with CLP. Irrespective of the fact that there are cleft centers where the parents are guided by the cleft teams, ultrasonographers, including radiologists and obstetricians-gynecologists, are often the experts who confront prospective parents and provide first information as soon as a diagnosis of CLP is confirmed.
Previous studies have suggested that early prenatal counseling should provide clear and consistent information on CLP, possible treatments, and prognosis to reduce anxiety, confusion, and uncertainty, which was believed to alleviate parents' worries and lower the risk of termination of pregnancy. 17, 24, 25, 26
Another study by J. Kuttenberger et al., 27 in 2010 evaluated parents' experiences with first counseling at a cleft center, focusing on timing, content, and quality of information provided after detecting CLP. The study found that professionals provided the first information about the cleft immediately after birth, with 21% of cases coming from obstetricians. Whereas the result of the present study found that fifty-five (80.9%) obstetricians and forty-eight (92.3%) radiologists detected CLP in prenatal ultrasonography, with sixty-five (95.60%) obstetricians and fifty (96.20%) radiologists indicating a high detection rate. Additionally, fifty-four (79.40%) obstetricians and twenty-three (44.20%) radiologists provided the first information to parents following prenatal cleft diagnosis. This makes it essential and crucial for them to have sufficient understanding and knowledge regarding the anomaly, which enables them to provide better first information regarding a multidisciplinary approach, including timely referral to an orthodontist specializing in cleft care.
According to Matsuo et al., 28 the newborn cartilage tissues are softer and more plastic due to increased estrogen levels from the mother. This plasticity allows for the reshaping of fragments, which lasts until 3-4 months, after which estrogen levels decrease and cartilage regains elasticity, making presurgical orthopedics crucial as soon as after birth. Early presurgical infant orthopedics, when used with surgical lip repair, enables a single initial surgery to address the nose, lip, and alveolar complex, reducing the need for secondary surgery. 29
In 2022, Kurt Demirsoy K evaluated the knowledge and awareness of obstetrician-gynecologists (OB-GYNs) about presurgical orthopedic treatment (NAM) for newborns with CLP. 23% referred newborns for NAM, while 77% did not. Of the 141 OB-GYNs, 42% had never heard of NAM treatment for CLP. 27% had information about NAM, while 73% did not know its purpose. The study highlights the need for increased awareness and education in this area. 30
While our study showed sixty-one (89.70%) obstetricians and forty-six (88.50%) radiologists were unaware of pre-surgical infant orthopedics, in comparison sixty (88.20%) obstetricians and forty-eight (92.30%) radiologists did not know NAM / LATHAM procedures. The success of presurgical orthopedic treatment is closely linked to its commencement as soon as possible after birth, requiring careful consideration of these ratios.
A study by Bocian and Kaback emphasizes that initial counseling is the most crucial stage for the development of parental adaptability. 31 The absence of clarity and misinformation among specialists can lead to confusion about a baby's future among parents, causing guilt and pressure and potentially leading to elective pregnancy termination. Sixty (88.20%) obstetricians and forty-two (80.80%) radiologists preferred to refer parents for proper counseling regarding the condition, however, there are ambivalent opinions among professionals over whom to refer the parent for the same.
To deliver appropriate information regarding clefts and avoid needless mother-child separation, J. Kuttenberger believes that continuous training and education for these specialists with the qualifications to provide initial information is crucial. 27
Our study revealed some interesting findings: 94.10% of obstetricians and 96.20% of radiologists prefer to have more knowledge on the management of CLP for their further practice and Overall awareness among the specialists on prenatal diagnosis of CLP using ultrasonography was high, whereas overall knowledge among the specialists on presurgical infant orthopedics, including NAM and LATHAM, was minimal and showed an overall positive attitude to have further knowledge on the same.
The study had a few limitations that might be attributed to the fact that a wider sample, including specialists from various countries and other specialties, could have been included. Larger sample sizes, higher participation rates, and worldwide involvement should be prioritized in future investigations.
Conclusion
Timely interventions along with a multidisciplinary approach of CLP, including specialists involved in diagnosis, early presurgical infant orthopedics, surgeries, and supportive care provide better aesthetic and functional outcomes. In the present study, it was shown that the awareness and attitude among the OB-GYNs, and radiologists on prenatal detection of CLP was found to be highly significant while there was limited knowledge among these specialists about CLP and its management.
However, to ensure that decisions are made in the best possible way, it is crucial to increase further the knowledge, awareness, and attitude among various medical specialists about evolving concepts, advanced technologies, newer procedures, and interventions in which the orthodontist will also play a significant role in the success of diagnosis and management of CLP.