Introduction
In everyday orthodontic practice, Class II malocclusion stands out as the prevailing skeletal misalignment frequently encountered, presenting in approximately 38% to 50% of clinical cases. This condition significantly impacts both the facial and dental aesthetics of individuals seeking orthodontic treatment.1 Historically, addressing these cases involved employing extraction therapy or employing techniques such as distalizing the maxillary molars through various intra-oral and or extra-oral techniques. However, these approaches often came with unintentional responsive forces, causing protrusion and anterior teeth moving forward movement, which is not ideal.2, 3, 4, 5 The mechanics of orthodontic treatment have undergone fundamental transformation due to introduction of TASDs i.e. Temporary Skeletal Anchorage Devices. A significant impact stemmed from Infra-zygomatic crest (IZC) bone screws which are a type of Extra-alveolar implants offering a convincing alternative for creating skeletal anchorage in the process of distalizing molars.6 Besides furnishing a dense cortical plate the IZC ridge is deemed optimal for implant insertion owing to its location being buccal thus away from root apices. Also this facilitates implant placement at higher level in the vestibule of maxilla along with seamless single-phase of unobstructed tooth movement when teeth are being retracted. These characteristics have significantly played a role in the notable 93.7% successful outcome of IZC implants.7
Clinically, the prominence of the zygomatic crest can be palpated along the buccal curve in between the maxillary alveolar process and zygomatic process. At the same time, it's important to note age-related variations; typically, in younger individuals, the ridge is found between the second premolar of maxilla and first molar of maxilla, while in adults, it tends to be positioned above the maxillary first molar.8
Lin supports Interdental Zygomatic Crest bone screws placement within the first and second molar region. In contrast, Liou favours a positioning that is more anterior, specifically in close proximity to the mesiobuccal root of the first molar tooth. 9 The suggested specifications for the IZC bone screw entail a size of 2×12 mm, crafted from stainless steel. The clearance between screw head and soft tissue which supports it is recommended to be 5mm for promoting better hygiene and preventing irritation of soft tissue. 10 The process of inserting the IZC bone screw includes an primary step of insertion of implant tip in the cortical bone positioned perpendicular to the long axis of the tooth structure. Subsequently, the screw is gradually oriented to approximately 55-70◦ below the horizontal plane. This aims to optimally engage the buccal bone. 7
Case report
This case report aims to emphasize the extent of distalization of maxillary arch achieved through the utilization of IZC bone screws in conjunction with a power arm hook of medium length (8-10mm).
A patient aged 24 year, female presented to the postgraduate clinic with the main concern of upper teeth protrusion. The patients’ past medical or dental history did not show any significant findings. There was no gross facial asymmetry on extra-oral examination. The profile of the patient was convex having posterior divergence. The lips were incompetent and mento-labial sulcus angle was deep.
Table 1
Cephalometric changes recorded after 6-months of IZC distalization procedure
Intra-oral examination
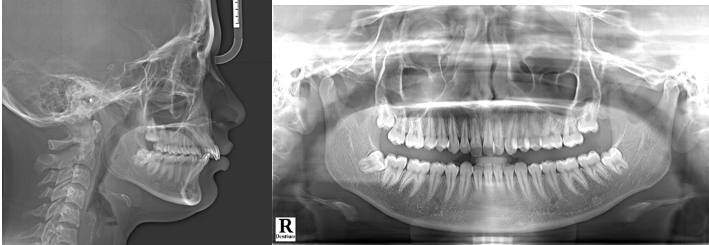
Upon examination, the patient displayed a full-cusp Class II molar relation on right and left sides and an end-on canine relation both side. There was no midline deviation and overjet measured 5 mm. The incisor exposure was increased by 5 mm. The proclination was observed in maxillary incisors while mandibular anterior teeth displayed mild crowding. No abnormality or pathology was observed in temporomandibular joint. (Figure 1).
The detailed analysis of lateral cephalogram disclosed that growth pattern was average (Figure 2) (Go-Gn-SN = 30º). The was maxillary excess in sagittal plane (SNA = 86º), and the mandible was retrognathic (SNB = 77º). The skeletal base was Class II pattern (ANB = 9º and Wits Appraisal = +7mm). Additionally, the analysis indicated proclination of maxillary incisors (Upper Incisor to NA = 31◦) along with relative mandibular incisors proclination (Lower Incisor to NB = 28º). The analysis of models demonstrated a Bolton’s ratio, indicating an excess of 1.8mm tooth material in mandibular anterior and overall mandibular excess (0.2mm).
Treatment objectives
The purpose of treatment was to enhance facial aesthetics by implementing the following strategies: distalizing the maxillary arch to address the 3 mm excessive overjet and correct the 3 mm arch length-tooth material discrepancy. The goal was reduction in protrusion of lips, attaining competency of lips, correction of overjet, and establishment of Class I molar and canine relation.
Furthermore, the objective was to attain an intrusion of more than 2 mm to counterbalance incisors that were seen excessively.
Treatment alternatives
Considering the patient's post-pubertal age, three distinct treatment strategies were recommended and outlined for the patient:
Surgical Intervention: The suggested course involved decompensation done orthodontically and orthognathic surgrey i.e. Lefort I Osteotomy involving the impaction of the maxilla posteriorly along with Bilateral Sagittal Split Osteotomy (BSSO) and advancing the mandible to address discrepancy in sagittal plane identified based on Burstone Analysis. (values: N-A-Pogonion = +23◦, Articular-Ptm(HP) = 30 mm, N-A (HP) = + 6 mm), N-B (HP) = - 15mm, PNS-ANS (HP) = 61 mm, Gonial- Pogonion = 74 mm, B-Pogonion (MP) = - 4 mm).
Premolar Extraction Approach: The recommended strategy involved camouflaging orthodontically by extracting maxillary first premolar and second premolar in mandible.
Distalization of complete arch and extraction of third molar: The chosen course of action involved an Orthodontic Camouflage approach, entailing maxillary third molar extractions. Additionally, total maxillary arch distalization to be achieved using IZC bone screws complemented by reduction of tooth material reduction in mandible through methods extraction of single incisor or inter-proximal stripping. Among all the available treatment choices, this approach stood out as the most conservative option.
Treatment plan
The treatment plan prioritized maximum maxillary arch distalization along with the teeth to enhance skeletal and dental parameters and soft tissue attributes. Essential components of the plan included the maxillary dentition alignment and levelling, coupled with correction of torque for the anterior maxillary teeth. This correction allowed for sufficient flexibility to facilitate posterior total arch displacement.
Treatment progress
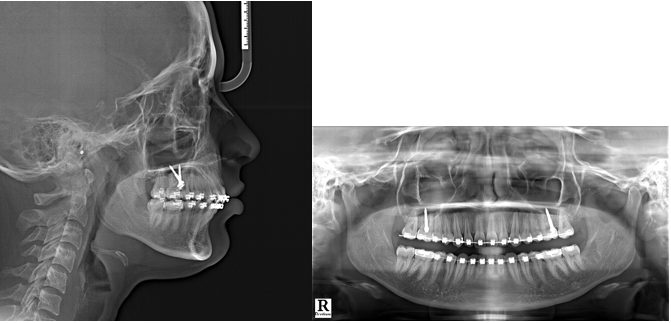
Extraction was performed for teeth 18 and 28, followed by the placement of bands on the first molars in maxilla and mandible, along with the attachment of bonded buccal tubes to second molars in maxilla and mandible. The Damon 0.022" × 0.028" slot metal bracket system by Ormco was utilized. Following the initial phase of leveling and alignment, 19 × 25 stainless steel archwires were introduced in maxilla and mandible. Additionally, 2 stainless steel IZC bone screws (Model: A1P-212012) measuring 2 × 12 mm by Bio-Ray® were strategically positioned in the zygomatic crestal bone in between the first and second maxillary molars on both sides, inclined at an angle of approximately 70 degrees and positioned 9 mm above the cemento-enamel junction.
A figure-of-eight steel ligature wire was employed to create a unified structure spanning across all maxillary teeth, ensuring even distribution of applied forces. A hook of medium-length (8-10mm) was secured on both sides of the maxillary archwire placed distally to the canine. This hook was then connected to the IZC bone screw with a 5mm-long Elastomeric chain, applying a force of 300 grams (10 oz) for distalization (Figure 4, 5).
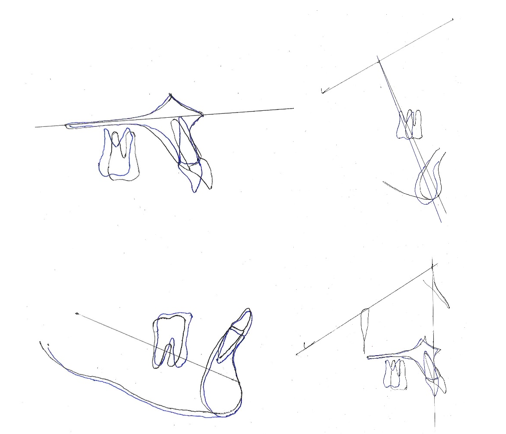
Taking into account the biomechanical implications, careful attention was given to maintaining the force vector's direction and height at or above the Cres of the maxillary dentition. This strategic approach aimed to induce bodily displacement along with rotation in counter-clockwise direction of the entire dentition and skeletal base. The treatment progressed for a period of 9 months; but as the patient had to relocate permanently to other location she had to regrettably discontinue the treatment. However, the treatment outcomes attained until this juncture have been thoroughly recorded in the following section detailing the results.
Treatment results
Positive changes were noted in both skeletal and dental parameters. The sagittal skeletal disparity showed enhancement, as indicated by the posterior shift of Point A and a decrease in the ANB angle by 3 degrees. Vertical angulation was slightly reduced further stating mandible undergoing forward auto-rotation and maxilla exhibiting intrusion.
Increase in the axial inclination of the maxillary anterior teeth expressed optimal torque articulation facilitated by the use of sequential archwires. Radiographic Analysis were used to measure molar distalization. (Figure 6).11 The application of distalizing forces resulted in approximately 3.5mm disatlization of maxillary molar (measured from U6 to Pterigoid vertical and U6 to Facial axis). This was clinically verified by the transition from a full cusp Class II to a Class I molar relation. The lack of change in axial inclination was evidenced by the degree of tipping (α angle) and U6 to True Vertical Line (cusp tip and root apex) (Table 1).
Following the post-distalization phase, settling elastics were administered and adjusted in accordance with ABO (American Board of Orthodontics) guidelines. Subsequently, the orthodontic appliance was removed through the debonding process (Figure 7).
Discussion
Facial aesthetics holds paramount importance for the majority of orthodontic patients, particularly when the degree of protrusion is moderate. In such cases, multiple extractions of maxillary and mandibular teeth is not patients’ choice. Although, if deemed necessary, they easily accept extraction of third molars due to their limited impact on both aesthetics and function. This readiness derives from the realization that removing third molars can free up space distal to the second molars, allowing for overall dentition distalization with the help of skeletal anchoring.13 The Cres for the entire maxillary skeletal base is located along the mesial face of the second premolar, around 8-10 mm from the cementoenamel junction (CEJ). 12, 13, 14, 15
According to Teuscher (1986), the Cres for the maxillary dentition is positioned between the roots of the two premolars, while the Cres of the maxilla itself is located in the posterosuperior region of the zygomaticomaxillary suture.15
Similarly, Jeong et al. (2009) showed in a finite element study that the Cres for the entire maxillary dentition was placed 26.5 mm posteriorly and 11.0 mm apically from the incisal edge of the upper central incisor, respectively. 16
If retraction forces traverse beneath the Cres of the maxillary dentition, it often leads to clockwise rotation of the anterior teeth, causing torque loss and exerting a vertical extrusion force on the incisors. 17 It is necessary to provide a increase positive crown torque in the anterior region of the rectangular archwire in order to compensate for this effect. 18
According to Hedayati et al., a 9 mm lever arm reduces the chance of anterior tooth rotation while also causing body movement regardless of whether the implant is placed distal or mesially relative to the premolar. 19 Therefore, the amount and direction of the force applied in relation to the Cres of the maxillary bone base are critical elements in accomplishing complete arch distalization. 20 The biomechanics and the particulars of the ensuing tooth movement are mostly determined by the height of the implant location and the length of the power arm. 21, 22, 23 Considering these factors, we opted for a hook of medium-length (8-10 mm) positioned distal to the maxillary canine. This placement aimed to achieve the closest proximity and optimal alignment of the point and line of action of force concerning the Centre of resistance of the maxillary dentition.
A significant limitation of intra-alveolar implant placement, according to Kuroda et al., is the increased risk of root approximation, impeding intended tooth movement and leading to premature contact with the implant. To overcome this challenge, the placement of implants in extra-alveolar regions, such as the IZC and Mandibular Buccal Shelf (MBS) bone screws, proves advantageous. 24 Implant stability is dependent on both quality (bone density) and quantity (bone volume). To guarantee safe loading, the effective biomechanics of IZC implants must be within permissible limits, as measured by bone density and volume, as exceeding these values may impair stability.25, 26
Conclusion
Concerning the force's line of action, magnitude, and point of application relative to the Cres of the maxillary dentoalveolar complex, along with the strategic extra-radicular positioning of IZC implants, achieving desired biomechanical outcomes is feasible, even in borderline surgical cases. This approach facilitates bodily distalization of the maxillary dentition with minimal tipping by utilizing forces in close proximity to the Cres. Consequently, this helps eliminate undesired effects of reactionary forces on the occlusal plane. A comprehensive understanding of biomechanics and its practical clinical application emerges as a cornerstone in devising effective orthodontic treatment strategies.