- Visibility 118 Views
- Downloads 13 Downloads
- DOI 10.18231/j.jco.2024.048
-
CrossMark
- Citation
Stability of skeletal open bite correction in adult patients by molar intrusion: A meta analysis
Introduction
Anterior open bite (AOB) malocclusion is the lack of vertical overlap or contact between the maxillary and mandibular incisors and is of multifactorial etiology.[1]
Skeletal anterior open bite is a discrepancy in the vertical plane of space effecting the jaw bases with a prevalence of 1.5% to 11% varying amongst ethnic groups.[2] Clinical Signs and symptoms of skeletal open bite being speech problems, unattractive smile, and difficulty biting food with front teeth., anterior open bite, lisping, increased lower anterior facial height.
Diagnosis of skeletal open bite requires precise clinical examination and cephalometric analysis.
Lateral cephalogram is one of the most common accessory diagnostic aid in diagnosing & treatment planning. Common cephalometric variables associated with skeletal open bite are: Skeletal parameters - decreased mandibular, increased mandibular plane angle, vertical downward position of maxilla and mandible in relation to cranial base, cranial cant of occlusal plane and increased anti inclination angle. Dental parameters - absence of overbite, increased molar distance from the palatal plane/mandibular plane.
Various modalities for treating skeletal open bite have been proposed which include surgical methods and non-surgical method. Surgical Treatment modalities for correcting skeletal open are invasive in nature and need not be always performed unless the skeletal malocclusion is severe in extent. Other treatment modalities for correcting open bites include reducing the posterior dentoalveolar height by applying intrusive forces to posterior teeth with Temporary Anchorage Devices. Posterior bite blocks can also be used to correct anterior open bites. [3], [4] Bite blocks augmented with magnetic augmentation [5], [6], [7] or springs [8] have also been used. Multi-loop edgewise arch wire techniques can be used. [9], [10]
Open bite is considered a malocclusion that still defies correction, especially in terms of stability. One might expect even more relapse and greater problems in treating open-bite malocclusions in adults. [11], [12] Growth in the vertical dimension is the last to cease, making corrections more prone to relapse. Correcting a skeletal open bite by molar intrusion has been found to be promising. However correcting a skeletal discrepancy by dentoalveolar means can be challenging from post retention point of view.
Clockwise rotation of the lower jaw is a result of more vertical growth at the molar region than at the mandibular condyles. [13] The rotations of the mandible can be affected by the dentoalveolar region hence if we alter the position of the molars in the vertical dimension, we can affect the current position of the mandible.
In this review, we compiled evidence from the articles on the long-term stability of the major therapeutic interventions for correcting anterior open bite.
The aim of this study is a systematic search for eligible publications and to conduct a meta-analysis regarding (1) Efficiency (2) Stability (3) Overall treatment time (4) Effectiveness of skeletal open bite treated with molar intrusion in adult patients.
Materials and Methods
Protocol and registration
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were followed to ensure transparency and comprehensiveness in this systematic review.
Eligibility criteria
The selection criteria according to PICOS was applied for this review are as presented in[Table 1].
Information sources, search strategy, and study selection
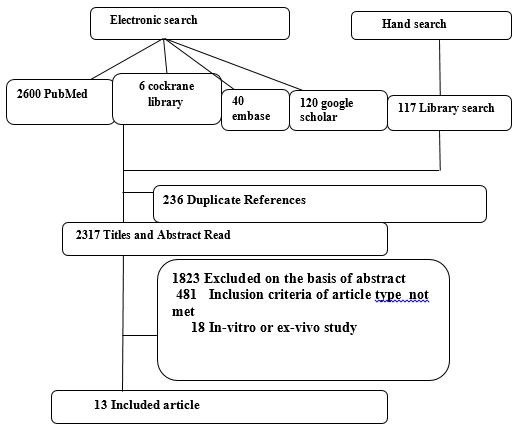
Electronic databases were searched, no limitation was put on the year of study publication. Cochrane Central Register of Controlled Trials (Central), PubMed, Embase and Google Scholar were searched. [Figure 1].The keywords used are as follows:- Skeletal openbite OR skeletal open bite AND molar intrusion OR intrusion of molars AND stability OR reliability NOT surgically treatment NOT surgically corrected NOT corrected by surgery NOT by extrusion of incisors.The article search, inclusion of study, method, assessment of quality, and data extraction were done by two reviewers individually and in duplicate .These reviewers were not blinded to the concerned authors. The results were revised by the second and fourth authors.Eligible articles were assessed in 2 phases. Only titles and abstracts were screened in the first phase. In the second phase assessment of full text was conducted for final eligibility. The articles which did not meet 1 or more of the inclusion criteria, were excluded.
Data collection process and data items
Two reviewers performed data extraction independently and in duplicate. Standardized data extraction sheets were used to perform data extraction.
Risk of bias (ROB) and quality assessment in individual studies
ROBINS-1[14] tool was used for quality assessment of the studies ([Table 2]). Seven components of bias were evaluated: (1) ] confounding bias , (2) Bias due to Inclusion of participants, (3) Bias due to classification of interventions (4) Bias arising from deviating from intended interventions/methods, (5) Bias due to loss of data, (6) Bias due to outcome measurements and (7) Bias due to reported result selection. For each included study, an overall assessment of bias (high, unclear, low) was made. Having at least one component was regarded as having an overall high ROB and that particular study/studies were excluded from the meta-analysis.
ROB across studies
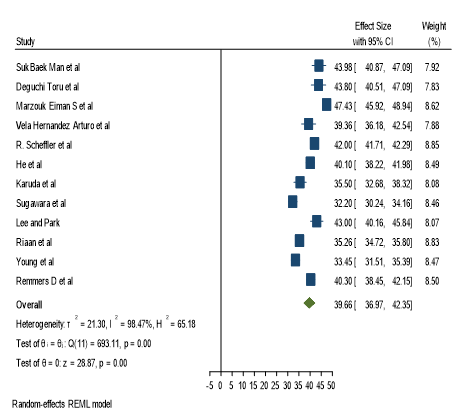
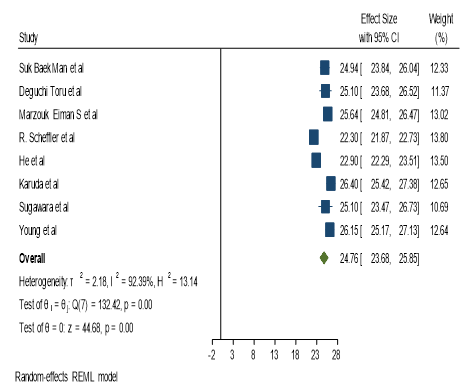
Standard forest plot/ funnel plots would be drawn using three specific parameters (overbite in mm, U6 -pp and SN MP Angle) for the studies that would be included in the meta-analysis.
Summary measures and synthesis of results
Otherwise, the results were qualitatively summarized. Chi-square test was used to explore Statistical heterogeneity with the I2 index, corresponding to less, moderate, and extremely high heterogeneity, with values of 25 percent, 5 percent, and 75 percent respectively. I2 test specified that the fixed-effects model and the random-effects model have to be applied to studies with more than 50% heterogeneity or 50% heterogeneity, respectively.
Additional analysis
|
Category |
Inclusion criteria |
Exclusion criteria |
|
Study design |
MRCT, Pre-post studies |
Case report |
|
Participants |
Healthy male and female patients, aged 18 years and above having skeletal open bite |
Unhealthy male and female patients, aged below 18 years having dentoalveolar open bite |
|
Intervention |
Molar Intrusion |
Extrusion of incisors, Surgical correction |
|
Control |
Extrusion of incisors, Surgical correction or conventional orthodontic therapy |
Molar Intrusion |
|
Outcome measures |
Primary outcomes-Stability of the skeletal open bite (OB in mm)( in percentage) treated with molar intrusion Secondary outcome-Whether the relapse in the overbite is Skeletal or dentoalveolar in nature |
|
|
Others |
English articles in which the studies have been performed on Human being |
Non English articles in which the studies have been performed on Human being/Animals |
|
S. No |
Study |
Pre-intervention |
At intervention |
Post-intervention |
||||
|
|
|
Bias due to confounding |
Bias in selection of participants into the study |
Bias in classifica on of inter- ventions |
Bias due to deviations from intended interventions |
Bias due to missing data |
Bias in measu- rement of outcomes |
Bias in selection of the reported result |
|
1 |
Suk Baek Man et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
2 |
Deguchi Toru et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
3 |
Marzo uk Eiman S et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
4 |
Vela Hernandez Arturo et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
5 |
R. Scheffler et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
6 |
He et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
7 |
Karuda et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
8 |
Sugawara et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
9 |
Lee and Park |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
10 |
Riaan et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
11 |
Young et al |
UNCLEAR |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
12 |
Remmers D et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
13 |
Geron et al |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
LOW |
|
S. No |
Search engines |
|
Results |
Final |
|
1 |
Central (The Cochrane Library) |
Skeletal openbite OR skeletal open bite AND molar intrusion OR intrusion of molars AND stability OR reliability NOT surgically treatment NOT surgically corrected NOT corrected by surgery NOT by extrusion of incisors |
6 |
1 |
|
2 |
Embase |
Same as above |
40 |
4 |
|
3 |
PubMed |
Same as above |
2600 |
7 |
|
4 |
Google Scholar |
Same as above |
120 |
1 |
|
Remmers D et al |
52 |
17.1 |
1.3 |
40.9 |
6.1 |
-3.2 |
1.9 |
|
|
0.4 |
1.1 |
40.6 |
6.3 |
|
|
5 |
0.2 |
1.8 |
40.3 |
6.8 |
|
|
|
Young et al |
29 |
26 |
1 |
32.73 |
6.45 |
–2.23 |
2.1 |
26.08 |
2.51 |
1.78 |
0.84 |
32.58 |
5.61 |
25.42 |
2.62 |
2 |
1.53 |
1.09 |
33.45 |
5.06 |
26.15 |
2.56 |
|
Geron et al |
39 |
27.23 |
6.38 |
|
|
-2.2 |
1.9 |
20.6 |
2.3 |
0.98 |
0.57 |
|
|
17.7 |
2.4 |
2 |
0.91 |
0.4 |
|
|
18.57 |
|
|
Riaan et al |
16 |
13.1 |
|
36.1 |
4.9 |
-2.2 |
1.7 |
|
|
0.8 |
1.1 |
34.9 |
5.3 |
|
|
1 |
0.56 |
1.1 |
35.26 |
1.1 |
|
|
|
Lee and Park |
11 |
18 |
|
44.9 |
3.9 |
-3.7 |
1.7 |
|
|
1.7 |
0.7 |
42.9 |
4.5 |
|
|
1.54 |
0.7 |
0.7 |
43 |
4.8 |
|
|
|
Sugawara et al |
9 |
19 |
|
33.1 |
2.1 |
-2.8 |
1.8 |
24 |
3 |
2.1 |
0.8 |
31.7 |
2.4 |
25 |
2.8 |
1 |
1.2 |
0.8 |
32.2 |
3 |
25.1 |
2.5 |
|
Karuda et al |
23 |
21.6 |
7.3 |
38.8 |
6.4 |
-5.2 |
1.8 |
28.7 |
2.8 |
1.5 |
0.6 |
35.5 |
6.9 |
26.4 |
2.4 |
2 |
1.5 |
0.6 |
35.5 |
6.9 |
26.4 |
2.4 |
|
He et al |
20 |
20.6 |
4 |
39.6 |
4.3 |
-1 |
1.6 |
22.7 |
1.4 |
2.1 |
1.1 |
40.1 |
4.3 |
22.9 |
1.4 |
1 |
2 |
1.1 |
40.1 |
4.3 |
22.9 |
1.4 |
|
R. Scheffler et al |
30 |
24.1 |
10.7 |
43 |
1 |
-1.5 |
1.6 |
24 |
1.4 |
0.7 |
1.3 |
42 |
1 |
21.7 |
1.1 |
2 |
0.3 |
1.1 |
42 |
0.8 |
22.3 |
1.2 |
|
Vela Herna´ndeza Arturo et al |
31 |
26.6 |
4.9 |
40.38 |
9.29 |
-2.48 |
1.57 |
|
|
1.5 |
0.47 |
39.19 |
8.98 |
|
|
2.8 |
0.94 |
0.57 |
39.36 |
9.04 |
|
|
|
Marzouk Eiman S et al |
26 |
33 |
|
49.05 |
3.9 |
-4.75 |
2.27 |
28.27 |
2.55 |
2.18 |
0.48 |
46.91 |
3.89 |
25.23 |
2.14 |
4 |
1.41 |
0.39 |
47.43 |
3.93 |
25.64 |
2.17 |
|
Deguchi Toru et al |
15 |
24.3 |
5.9 |
45.8 |
6 |
-4.4 |
1.2 |
26.9 |
3 |
1.8 |
1.1 |
42.2 |
6.7 |
24.6 |
2.5 |
2 |
1 |
0.9 |
43.8 |
6.5 |
25.1 |
2.8 |
|
Suk Baek Man et al |
9 |
23.7 |
26.41 |
45.44 |
4.11 |
-3.91 |
1.65 |
26.88 |
1.12 |
1.65 |
0.82 |
43.41 |
4.41 |
24.5 |
1.64 |
4 |
0.45 |
1.09 |
43.98 |
4.76 |
24.94 |
1.68 |
|
|
|
at T1 |
age (y) |
SN-MP (degree) |
SN-MP SD |
OB (mm) |
OB SD |
U6-PP (mm) |
U6-PP SD |
OB (mm) |
OB SD |
SN-MP (degree) |
SN-MP SD |
U6-PP (mm) |
U6-PP SD |
time (y) |
OB (mm) |
OB SD |
SN-MP (degree) |
SN-MP SD |
U6-PP (mm) |
U6-PP SD |
|
Study |
T1 (n) |
Age (y) |
SD |
T1 |
T1 |
T1 |
T1 |
TI |
T1 |
T2 |
T2 |
T2 |
T2 |
T2 |
T2 |
T3 F/U |
T3 |
T3 |
T3 |
T3 |
T3 |
T3 |
|
Post treatment Overbite (mm) |
Post retention Overbite (mm) |
Difference |
Percentage of Stability |
Percentage Of Relapse |
Significance |
|
1.47 |
1 |
0.47 |
68% |
32% |
P<0.002 |
|
Post treatment SN MP Angle (degree) |
Post retention SN MP Angle (degree) |
Difference |
Percentage of Stability |
Percentage of relapse |
Significance |
|
39.33 |
39.66 |
0.33 |
99% |
1% |
p=0.065 |
|
Post treatment SN MP Angle (degree) |
Post retention SN MP Angle (degree) |
Difference |
Percentage of Stability |
Percentage of relapse |
Significance |
|
39.33 |
39.66 |
0.33 |
99% |
1% |
p=0.065 |
|
Post treatment U6 PP (mm) |
Post retention U6 PP (mm) |
Difference |
Percentage of Stability |
Percentage of Relapse |
Significance |
|
23.69 |
24.76 |
1.07 |
95% |
5% |
p<0.0024 |
Result
Study selection and characteristics
2883 articles were found using electronic search and hand search, out of which 566 were duplicates and were excluded. 2317 articles remained and their titles and abstracts were read. On the basis of abstract, 1823 articles were excluded. On the basis of inclusion criteria 450 articles were excluded.6 articles were found to be ex vivo studies and were excluded.
Hand search was also on the reference lists of the retrieved full articles. The complete search and data retrieval was independently performed by at least 1 investigator. In case, there was any confusion, a second investigator was called.
44 randomized controlled trials were included for the qualitative analysis. Only 13 studies were included in the quantitative synthesis. 31 studies included in the qualitative synthesis were case reports.
Study characteristics and ROB within studies
Titles and Abstracts of potential articles for inclusion criteria were examined; the articles were included based on consensus agreement.
The articles that were included are as follows: - Suk Baek Man et al, [15] Deguchi Toru et al., [16] Marzo uk Eiman S et al, [17] Vela Hernandez Arturo et al, [18] R. Scheffler et al., [19] He et al, [20] Karuda et al [21] Sugawara et al, [22] Lee and Park, [23] Riaan et al, [24] Young et al, [25] Remmers D et al, [26] Geron et al. [27]
The characteristics of all the included studies are given in [Table 3].
After compiling the articles to be included, articles were read and the data was abstracted onto custom data abstraction forms, which was pre-tested and piloted on 2 studies of each type. Abstracts of articles were examined, with the full article retrieved if necessary.
Thirteen studies were identified in the search forest plot graphs were plot for each parameter allowing extraction of mean OB, SN –MP angle and U6-PP angle for the pre intervention condition (T1), the post treatment result after therapeutic intervention (T2), and long-term stability follow-up (T3) These data were pooled to enable the primary evaluation of long-term s nonsurgical open-bite treatment outcomes by molar intrusion.
ROB within studies are given in [Table 2].
Results of individual studies
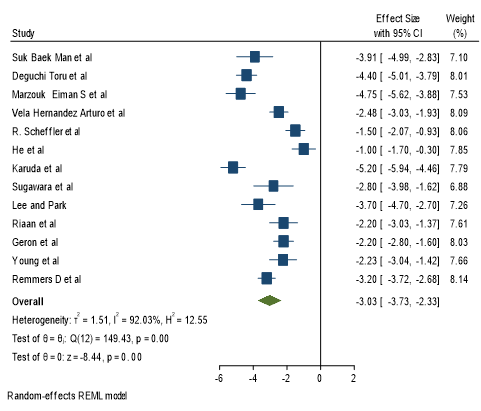
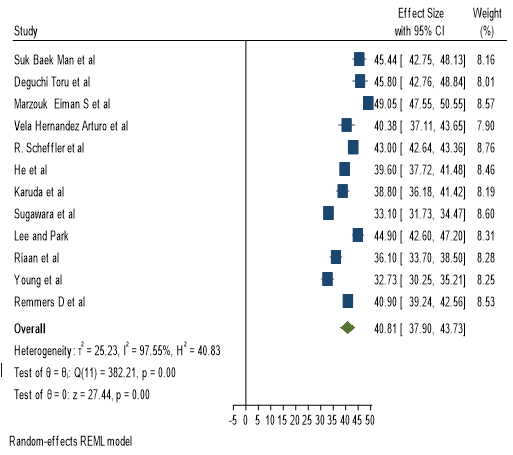
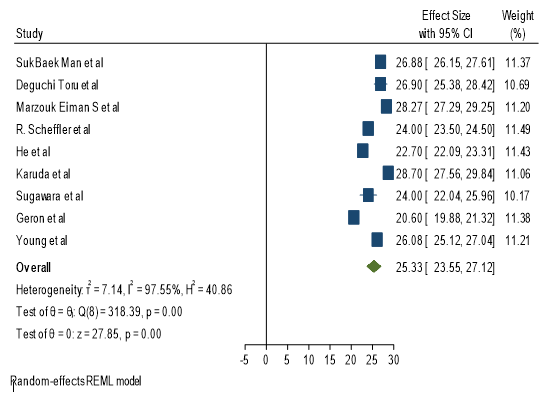
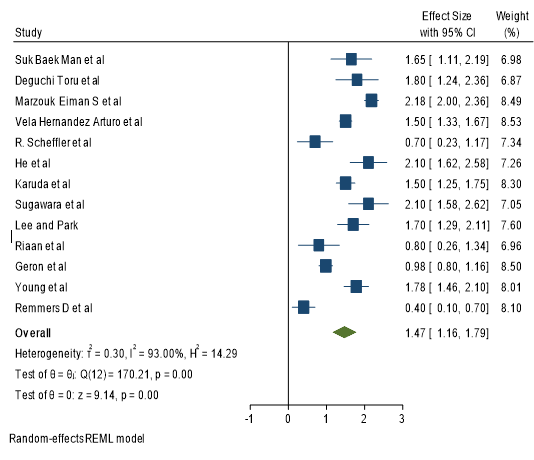
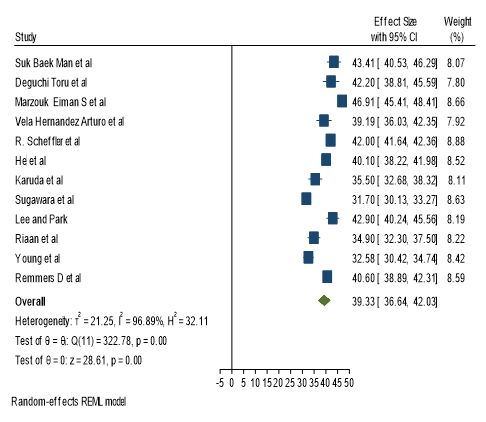
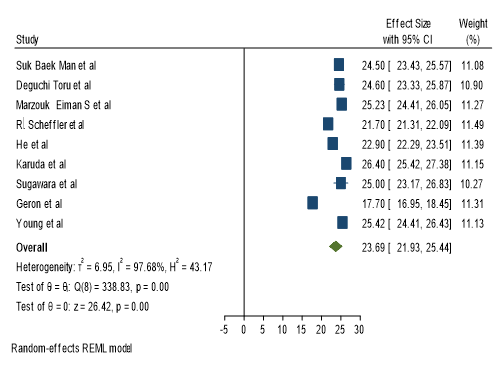
To calculate or primary outcome i.e. Stability of overbite correction, overbite (in mm) was taken as a parameter. This parameter was fond in all 13 articles[Figure 2],[Figure 3] and [Figure 4] F tells us the overall mean Pretreatment overbite (in mm), Pretreatment SN MP Angle and Pretreatment U6-PP plane (in mm). [Figure 5],[Figure 6] and [Figure 7] tells us the overall mean Post treatment overbite (in mm), Post treatment SN MP Angle and Post treatment U6-PP plane (in mm).
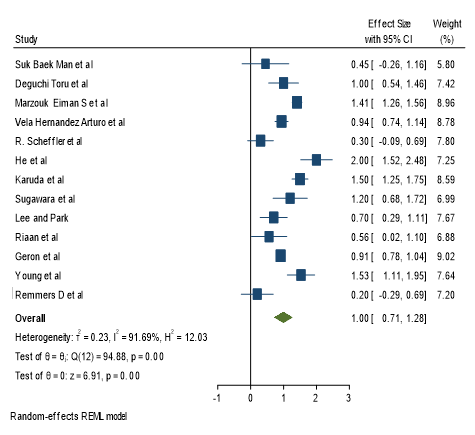
[Figure 8], [Figure 9] and [Figure 10] tells us the overall mean Post retention overbite (in mm), Post retention SN MP Angle and Post retention U6-PP plane (in mm).
Synthesis of results
On comparing pretreatment and post treatment values of overbite mean which was derived from their respective forest plot graphs ([Figure 2] and [Figure 5]), significant amount of correction in overbite was found.
On comparing pretreatment and post treatment values of SN MP angle mean which was derived from their respective forest plot graphs ([Figure 3] and [Figure 6]), significant amount of reduction in the angle was found.
The reason behind this was due to intrusion of the molars, this in turn leads to autorotation of the mandible in the anti-clockwise direction leading to a decrease in SN MP angle.[Figure 4] and [Figure 7]), significant amount of reduction in the parameter was found was found, indicating that the molars were intruded.On comparing post treatment(1.47mm) and post retention(1 mm) values of overbite which was derived from their respective forest plot graphs ([Figure 5] and [Figure 8]), significant amount of relapse was found.
To find out the cause of relapse, two more parameters were taken.[Figure 6] and [Figure 9]), non-significant amount of relapse was found.On comparing post treatment (23.69 mm) and post retention(24.76 mm) values of U6 PP (mm) which was derived from their respective forest plot graphs (Figure 7 and Figure 10 ), significant amount of relapse was found.
Rob across studies
The risk of bias across studies were low
Discussion
Summary of evidence
The different post retention time periods and absence of U6-pp values among the studies has led to increased level of heterogeneity. Nevertheless, this uncontrolled sample represents the best evidence to date and could serve as a starting point for future studies with more rigorous designs
According to [Table 4] significant change in Post retention Overbite (in mm) compared to post treatment Overbite (in mm) indicates the nature of the corrected overbite was subject to relapse.
According to [Table 5] no significant change in Post retention SN MP Angle compared to Post treatment SN MP Angle indicates that no residual disproportionate growth in the vertical dimension was left in the patient which would have been responsible for relapse. According to [Table 6], significant change in U6 pp indicates the nature of the relapse to be of dentoalveolar origin.
According to [Table 4], [Table 5], [Table 6] this study shows that skeletal open bite patients treated with molar intrusion have 68 % stability which is supported by [Table 4]. Whereas the molar which was intruded have a 95% stability which is supported by table 6. The findings confirm that there was no residual growth left in the patients and the relapse was dentoalveolar in nature as confirmed by [Table 5] and [Table 6]. Other studies in the past have concluded that correction of skeletal open bite has a relapse rate of approximately 25% to 30%. However they do not specify the relapse rate of skeletal open bite treated with different treatment modalities separately. Although a previous meta analysis was conducted which elaborated the overall stability of skeletal open bite, the nature of relapse, it been skeletal or dentoalveolar in nature has not been commented upon.
This study has attempted to rule out the reason of relapse to be dentoalveolar in nature and not skeletal. No Disproportionate residual growth was responsible for the bite to relapse as indicated by there been no significant change in the mean SN-MP angle of post treatment from that of post retention. This study was also aimed to co relate the rate of overbite relapse with that of the amount of relapse in molar intrusion. There are limitations to this analysis, mostly due to the low level of evidence of the included studies.
Of particular interest is clinical decision-making for borderline patients, such as older adolescents with AOB or adults with mild to moderate open bite
Limitations
Several shortcomings were observed because of the lack of adequate randomization methods, absence of outcome assessment blinding.
Conclusion
This study states that skeletal open bite patients treated with molar intrusion have 68 % stability, whereas the intruded molar have a 95% stability.
As discussed previously the reason why the mandible’s movement doesn’t follow a 1:1 ratio is because of its cantilever like anatomy.[2]
No residual disproportionate growth in the vertical dimension was left in the patient which would have been responsible for relapse and the relapse was dentoalveolar in nature.
Source of Funding
None.
Conflict of Interest
None.
References
- IL Nielsen. Vertical malocclusions: etiology, development,diagnosis and some aspects of treatment. Angle Orthod 1991. [Google Scholar]
- P Sandler, A Madahar, A Murra. Anterior open bite: aetiology and management. Dent Update 2011. [Google Scholar]
- HN Iscan, L Sarisoy. Comparison of the effects of passive posterior bite-blocks with different construction bites on the craniofacial and dentoalveolar structures. Am J Orthod Dentofac Orthop 1997. [Google Scholar]
- WR Proffit. . St Louis:Mosby Year Book 1993. [Google Scholar]
- A Breunig, T Rokosi. The treatment of open-bites using magnets. Fortschr Kieferorthop 1992. [Google Scholar]
- EL Dellinger. Active vertical corrector treatment-long-term follow-up of anterior open bite treated by the intrusion of posterior teeth. Am J Orthod Dentofac Orthop 1996. [Google Scholar]
- JH Noar, N Shell, NP Hunt. The performance of bonded magnets used in the treatment of anterior open bite. Am J Orthod Dentofac Orthop 1996. [Google Scholar]
- R Kuster, B Ingervall. The effect of treatment of skeletal open bite with two types of bite-blocks. Eur J Orthod 1992. [Google Scholar]
- YH Kim. Anterior openbite and its treatment with multiloop edgewise archwire. Angle Orthod 1987. [Google Scholar]
- YH Kim, UK Han, DD Lim, Mlp Serraon. Stability of anterior open bite correction with multiloop edgewise archwire therapy: a cephalometric follow-up study. Am J Orthod Dentofac Orthop 2000. [Google Scholar]
- GS Dyer, EF Harris, JL Vaden. Age effects on orthodontic treatment: adolescents contrasted with adults. Am J Orthod Dentofac Orthop 1991. [Google Scholar]
- BK Nieke. Retention and stability considerations for adult patients. Dent Clin North Am 1996. [Google Scholar]
- FF Schudy. The rotation of the mandible resulting from growth: its implications in orthodontic treatment. Angle Orthod 1965. [Google Scholar]
- J Sterne, MA Hernán, BC Reeves, J Savović, ND Berkman, M Viswanathan. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016. [Google Scholar]
- M Baek, Y Choi, H Yu, K Lee, J Kwak, Y Park. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofac Orthop 2010. [Google Scholar]
- T Deguchi, H Kurosaka, H Oikawa, S Kuroda, I Takahashi, T Yamashiro. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am J Orthod Dentofac Orthop 2011. [Google Scholar]
- E Marzouk, H Kassem. Evaluation of long-term stability of skeletal anterior open bite correction in adults treated with maxillary posterior segment intrusion using zygomatic miniplates. Am J Orthod Dentofac Orthop 2016. [Google Scholar]
- AV Hernández, RL García, VG Sanz, VP Gallardo, FL Latorre. Nonsurgical treatment of skeletal anterior open bite in adult patients: Posterior build-ups. Angle Orthod 2017. [Google Scholar]
- N Scheffler, W Proffit, C Phillips. Outcomes and stability in patients with anterior open bite and long anterior face height treated with temporary anchorage devices and a maxillary intrusion splint. Am J Orthod Dentofac Orthop 2014. [Google Scholar]
- S He, J Gao, P Wamalwa, Y Wang, S Zou, S Chen. Camouflage treatment of skeletal Class III malocclusion with multiloop edgewise arch wire and modified Class III elastics by maxillary mini-implant anchorage. Angle Orthod 2013. [Google Scholar]
- S Kuroda, Y Sakai, N Tamamura, T Deguchi, TT Yamamoto. Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes. Am J Orthod Dentofac Orthop 2007. [Google Scholar]
- J Sugawara, U Baik, M Umemori, I Takahashi, H Nagasaka, H Kawamura. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. . Int J Orthod Orthog Surg 2002. [Google Scholar]
- Y Park, H Lee, N Choi, D Kim. Open Bite Correction by Intrusion of Posterior Teeth with Miniscrews. The Angle Orthod 2008. [Google Scholar]
- R Foot, O Dalci, C Gonzales, N Tarraf, M Darendeliler. The short-term skeleto-dental effects of a new spring for the intrusion of maxillary posterior teeth in open bite patients. Prog Orthod 2014. [Google Scholar]
- Y Kim, U Han, D Lim, M Serraon. Stability of anterior openbite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am J Orthod Dentofac Orthop 2000. [Google Scholar]
- D Remmers, RV Hullenaar, E Bronkhorst, S Bergé, C Katsaros. Treatment results and long-term stability of anterior open bite malocclusion. Orthod Craniofac Res 2008. [Google Scholar]
- S Geron, A Wasserstein, Z Geron. Stability of anterior open bite correction of adults treated with lingual appliances. Eur J Orthod 2012. [Google Scholar]
- Introduction
- Materials and Methods
- Protocol and registration
- Eligibility criteria
- Information sources, search strategy, and study selection
- Data collection process and data items
- Risk of bias (ROB) and quality assessment in individual studies
- ROB across studies
- Summary measures and synthesis of results
- Additional analysis
- Result
- Study selection and characteristics
- Study characteristics and ROB within studies
- Results of individual studies
- Synthesis of results
- Rob across studies
- Discussion
- Limitations
- Conclusion
- Source of Funding
- Conflict of Interest
