- Visibility 251 Views
- Downloads 34 Downloads
- DOI 10.18231/j.jco.2024.054
-
CrossMark
- Citation
Occlusal splint therapy- myth or fact? -A case report
- Author Details:
-
Madhvi Bhardwaj *
-
Shantanu Khattri
-
Sourabh Dutta
-
Rajiv Ahluwalia
Introduction
TMDs consist of a group of intricate conditions which are not fully comprehended, leading to symptoms such as discomfort in the jaw area and its related muscles, as well as constraints in performing common functions like speaking, facial expressions, chewing, and swallowing. TMDs can have a variety of causes, from unknown sources to systemic medical disorders. [1] TMD is widely classified by the American Academy of Orofacial Pain into intra-articular and extra-articular categories. Both of these classifications can coexist, which complicates diagnosis and therapy (Kafas and Leeson, 2006). TMD is treated with a combination of conservative and surgical methods. Conservative therapies include a range of techniques including as physical therapy, splint therapy, external muscle massages, targeted steam applications, occlusal modifications, analgesic pain management, and jaw exercises. Other treatment options include diathermy, ultrasound, soft laser therapy, acupuncture, and infrared radiation. However, surgical techniques like meniscoplasty and meniscectomy, which frequently entail replacing the joint's disk with a Proplast-Teflon interpositional implant, can be used as therapies for TMD (Tolvanen et al., 1988, Peltola et al., 2000).[2]
An occlusal splint was utilized to treat a patient who had TMD brought on by occlusal discrepancy, as reported in this case study.
Case Report
The chief complaint of a 27-year-old male patient who presented to the Orthodontics and Dentofacial Orthopaedics department was discomfort in the left side of the head, neck, and shoulder, along with left eye dysfunction that had been present for five to six months. Patient also complained of frequent unilateral headache, feeling of stress and nasal blockage on the left side. There was no history of trauma injury to head, neck or jaw region. Patient gave history of painkiller medication since 1 year with symptomatic relief.
Examination
Clinical examination revealed discernment in eye movements on right and left side with restricted movement of left eye. Patient gave history of frequent pain in head, neck and shoulder region on the left side. Patient also had abnormal posture with strained neck and shoulder on the left side. On a clinical assessment for signs and symptoms of TMD, it was noted that the patient had unilateral clicking sound on right side and was unable to open his mouth beyond 48mm. A deviation was noted towards the right side during mouth opening. Lateral excursion movements of the mandible were recorded as 3mm on right side and 2mm on the left. On palpation of muscles of mastication, no tenderness was found and there was no TMJ crepitus detected on either of the sides.

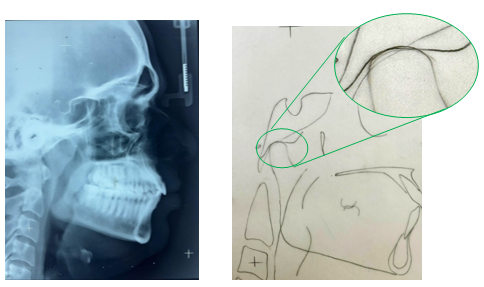
Radiographic interpretation
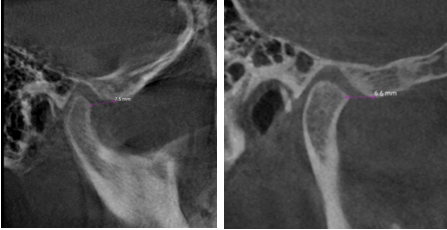
CBCT of the region of condyle revealed that it is angular in shape and demonstrated mild osteoarthritic degenerative joint changes with the appearance of mild erosion on the anterosuperior surface of the condyle and flattening of the head of the mandibular condyle on anatomic specimen. The distance between the articular eminence to the anterior most point of the condylar head was 7.5 mm on right side and 6.6 mm on left side. The posterior wall of the glenoid fossa's inferior most point was 3 mm on the right side and 3.2 mm on the left when measured linearly from the condylar wall.
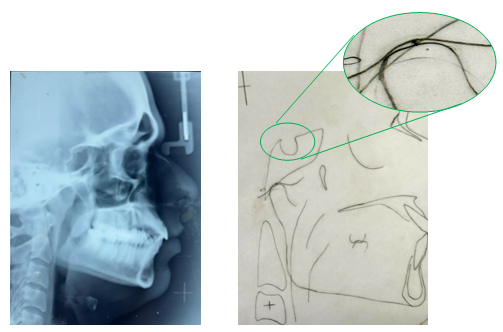
Cephalometric analysis showed saddle angle 127 °, distance of articular eminence to the anterior most point of condyle is 1mm and distance between the condylar wall and the posterior wall of the glenoid fossa's inferior most point is 2mm.
Diagnosis
Unilateral remodeled with parafunctionally adapted right condyle.
Differential diagnosis
Osteoarthritis with no disk derangement of right condyle
Treatment plan
Stabilising splint therapy for 6–8 months [3] was advised along with muscle exercises for 10-15 minutes/day. The patient was advised not to open his mouth wide.
Fabrication of splint
Impressions of the upper and lower arch was taken using alginate impression material. Type III orthodontic stone, Orthokal was used to pour the impressions. Retrieved models were then placed in vacuum forming machine and occlusal splints were adapted on the models with thermoplastic sheets of 1.5mm thickness. The splint was trimmed and borders smoothened so as to avoid any impingement of the appliance to the tissue. It was further adjusted in the patient’s mouth and the patient was instructed to wear the appliance full time.

Follow-up observations
The patient was recalled after 6 months of wearing the appliance. The patient reported decrease in frequency of headaches and neck pains. The pain in the left shoulder was also relieved. The patient reported that he no longer required the use of NSAIDs as prescribed before since 3 months. Eye pressure was also relieved which resulted in improved movement of the left eye and more coordinated eye movements bilaterally than before. The mouth opening improved and the maximum opening without pain was now recorded to be 62mm. There was no tenderness on palpation and crepitus recorded, although clicking sounds on the right side still persisted but were irregular.

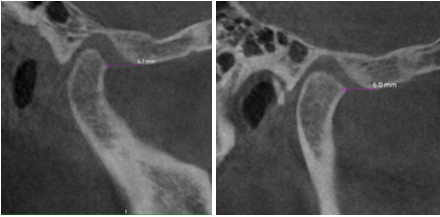
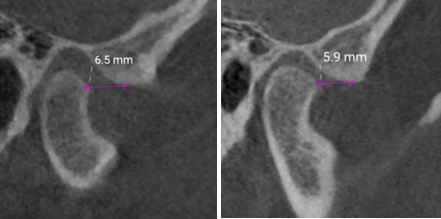
CBCT evaluation of the condyles after splint therapy showed that although the anterosuperior surface of the right condyle was flattened and minor erosion was also seen, there was increase in the joint spaces on the right side. The distance between the articular eminence to the anterior most point of the condylar head was found to be 6.7 mm of right side and 6 mm of left side, whereas the distance between inferior most point of the posterior wall of glenoid fossa to condylar head was 2.3mm and 3mm for right and left side respectively. The distances from the right and left articular eminence to the anterior most point of the condylar head and the posterior wall of the glenoid fossa's inferior most point to the condylar wall differed by 3.4 and 0.7 mm, respectively.
Follow up after 8 months, cephalometric analysis showed saddle angle 130 °, distance of articular eminence to the anterior most point of condyle is 0mm and distance between the condylar wall and the posterior wall of the glenoid fossa's inferior most point is 0mm.
|
CBCT scan parameters |
Pre-Treatment |
Follow Up After 6 Months |
Follow Up After 8 Months |
|
Distance of articular eminence to the anterior most point of condyle on right side. |
7.5 mm |
6.7 mm |
6.5 mm |
|
Distance between the right side condylar wall and the posterior wall of the glenoid fossa's inferior most point. |
3 mm |
3.3 mm |
3.5 mm |
|
Distance of articular eminence to the anterior most point of condyle on left side. |
6.6 mm |
6 mm |
5.9 mm |
|
Distance between the left condylar wall and the posterior wall of the glenoid fossa's inferior most point. |
3.2 mm |
3.5 mm |
3.7 mm |
|
Cephalometric parameters |
Pre-treatment |
Follow up after 8 months |
|
Saddle Angle |
127 ° |
130 ° |
|
Distance of articular eminence to the anterior most point of condyle. |
1mm |
0mm |
|
Distance between the condylar wall and the posterior wall of the glenoid fossa's inferior most point. |
2mm |
0mm |

Discussion
The patient presented with Osteoarthritic changes in the right condyle with alteration in shape accompanied with erosion and flattening of the right condylar head. Osteoarthritis patients frequently experience degenerative changes, which are difficult to reverse and manifest as alterations in the articular disc's mechanical characteristics (thinning and degradation), as well as morphologic changes in the shape of the condylar head and articular eminence. However, conservative treatment approach for treating pain associated with Osteoarthritis of TMJ is by Pharmacological approach for symptomatic relief and use of occlusal splint therapy and physiotherapy. Stabilization using occlusal splints has proven to reduce pain associated with TMD as they help to reduce TMJ loading. It has been proposed that physiotherapy plays a significant role in the treatment of TMD, and it may be especially helpful for myofascial pain or myalgia. It is crucial to comprehend the loading of the stomatognathic system and the presence of any stress or parafunctions while providing physiotherapy, including muscle training and behavior modification. [4], [5] Research shows that physiotherapy is useful in treating TMD, especially the headache symptoms connected to the illness. [6] According to Alkhutari et al., using an occlusal splint may enhance patient-centered treatment outcomes, indicating that this may be more than just a placebo effect. [7] There are several designs to choose from, including anterior repositioning splint, soft, and hard designs. Since the effectiveness of several occlusal splint designs has been shown in conflicting research, there is currently no agreement on which design is better. [8], [9] By creating stability, the ultimate purpose of splints and adjustments is to reduce discomfort in the masticatory muscles and joints. [10] In this case report, the morphologic changes of the condyle lead to compression of the muscles and downward displacement of the right condyle which lead to severe TMD associated pain in the head, neck and shoulder region on the left side. After 6 months of splint therapy accompanied with muscle exercises, due to relieve of occlusal load from the TMJ, significant improvement was recognized radiographically in the condylar region with increase in the joint spaces in the anterosuperior region where the linear distance between the articular eminence to the anterior most point of the condylar head increased from 6.8mm to 7.5mm in the right side and 3.9mm to 4.1mm in left side whereas the distance from the inferior most point of the glenoid fossa to posterior condylar wall decreased from 3mm to 2.3mm in right side and 3.2mm to 3mm in left side. Significant changes were also noted clinically with complete relief of pain from left shoulders, improved posture and decrease in the frequency of headaches and neck stiffness.
Conclusion
Proper functioning of the temporomandibular joint is essential to maintain and carry out the various functions of the stomatognathic system. Osteoarthiritis of the TMJ leads to various degenerative changes in the morphology of the joint which effects its proper functioning and leads to TMD associated symptoms. As presented in this case, use of gnathological splints also with exercises helps in relieving excessive stresses and load from the condyle thus allowing deprogramming of the muscles and better functional remodeling process of various structures of the temporomandibular joint which helped eliminate pain and significantly reduce other symptoms associated with TMD. Hence it is proved that occlusal splint therapy works.
Source of Funding
None.
Conflict of Interest
None.
References
- AG Pullinger, DA Seligman, WK Solberg. Temporomandibular disorders. Part II: Occlusal factors associated with temporomandibular joint tenderness and dysfunction. J Prosthet Dent 1988. [Google Scholar]
- SA Seifeldin, KA Elhayes. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs). Saudi Dent J 2015. [Google Scholar]
- J Okeson. . Orthodontics Current Principles and Techniques 2005. [Google Scholar]
- C Incorvati, A Romeo, A Fabrizi, L Defila, C Vanti, MRA Gatto. Effectiveness of physical therapy in addition to occlusal splint in myogenic temporomandibular disorders: Protocol of a randomised controlled trial. BMJ 2020. [Google Scholar]
- HA Van Der Meer, LB Calixtre, RH H Engelbert, CM Visscher, MW Nijhuis-Van Der Sanden, CM Speksnijder. Effects of physical therapy for temporomandibular disorders on headache pain intensity: A systematic review. Musculoskelet Sci Pract 2020. [Google Scholar]
- DT Li, YY Leung. Temporomandibular disorders: current concepts and controversies in diagnosis and management. Diagnostics 2021. [Google Scholar]
- AS Alkhutari, A Alyahya, PC Rodrigues Conti, N Christidis, EA Al-Moraissi. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J Prosthet Dent 2020. [Google Scholar]
- EA Al-Moraissi, R Farea, KA Qasem, MS Al-Wadeai, ME Al-Sabahi, GM Al-Iryani. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: Network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 2020. [Google Scholar]
- SA Seifeldin, KA Elhayes. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs). Saudi Dent. Saudi Dent J 2015. [Google Scholar]
- MK Murphy, R Macbarb, ME Wong, KA Athanasiou. Temporomandibular joint disorders: a review of etiology, clinical management, and tissue engineering strategies. . Int J Oral Maxillofac Imp 2013. [Google Scholar]
How to Cite This Article
Vancouver
Bhardwaj M, Khattri S, Dutta S, Ahluwalia R. Occlusal splint therapy- myth or fact? -A case report [Internet]. J Contemp Orthod. 2024 [cited 2025 Sep 09];8(3):365-369. Available from: https://doi.org/10.18231/j.jco.2024.054
APA
Bhardwaj, M., Khattri, S., Dutta, S., Ahluwalia, R. (2024). Occlusal splint therapy- myth or fact? -A case report. J Contemp Orthod, 8(3), 365-369. https://doi.org/10.18231/j.jco.2024.054
MLA
Bhardwaj, Madhvi, Khattri, Shantanu, Dutta, Sourabh, Ahluwalia, Rajiv. "Occlusal splint therapy- myth or fact? -A case report." J Contemp Orthod, vol. 8, no. 3, 2024, pp. 365-369. https://doi.org/10.18231/j.jco.2024.054
Chicago
Bhardwaj, M., Khattri, S., Dutta, S., Ahluwalia, R.. "Occlusal splint therapy- myth or fact? -A case report." J Contemp Orthod 8, no. 3 (2024): 365-369. https://doi.org/10.18231/j.jco.2024.054
