- Visibility 58 Views
- Downloads 20 Downloads
- DOI 10.18231/j.jco.2025.011
-
CrossMark
- Citation
Comparison of linear dimensional changes of mandibular symphyseal morphology in patients of various age groups with different growth patterns - A retrospective CBCT study
Introduction
The mandibular symphyseal morphology is a significant aspect of diagnosis and treatment planning in orthodontic treatment. It is essential in evaluating the profile of a patient and is an integral part of the mandibular anatomy. The mandibular symphyseal morphology being one of the predictors of mandibular growth rotation, the inclination of the symphysis is a decisive feature. In VGP, the symphysis protrudes forward in the face and the chin is prominent, while in the sagittal type, it is backwards, with a receding chin.[1] At the early age of 6–9 months, the fusion of the mandibular symphysis takes place and it continues to grow until adolescence. Several factors affect the symphyseal morphology including genetic, epigenetic and environmental factors. Functional demands dictate the masticatory force, which determines the fusion and remodeling of the symphysis. The various biomechanical loadings bring about adaptive morphological response.[2] Thus vertical jaw relationships and lower incisor proclination also influence the symphysis.[3]
Many methods have been used previously to examine the symphyseal morphology in humans such as dried skulls and conventional radiography. Conventional radiographic techniques only provide a two-dimensional image of three-dimensional structures leading to distortion, magnification, and error in identification. Recently developed CBCTs are an alternative to conventional CT which is cost-effective and allows for a lower radiation dose with a shorter scanning time.[4], [5] CBCT is capable of providing accurate images of the complex craniofacial region and has been used in several studies on the mandible and its morphometry.[6], [7]
The lower anteriors' orthodontic tooth movement is limited by the dentoalveolar symphysis's boundaries.[8] A change in lower anterior proclination will occur from orthodontic treatment used to dentally compensate for mild to moderate skeletal discrepancies.[9] Potential periodontal damage during tooth movement should be considered during treatment planning. A thorough examination of the morphology of the mandible's cross-section and the limitations of the bone is necessary to assess and reduce the risks of iatrogenic injury, such as dehiscence and fenestration during tooth movement. Therefore, the mandibular symphysis's dimensions can be a valuable diagnostic tool. [8]
Previously, lateral cephalograms were used to compare the symphyseal morphology in various vertical and anteroposterior relationships.[10] Studies on the variations of the symphysis seen in males and females concluded that symphysis was size-dependent and its size and shape were sex-independent.[11] There is no adequate scientific literature on the determination of symphyseal morphology in patients of various age groups with different growth patterns. The current research aimed at comparing the linear dimensional variations of the mandibular symphysis seen in various age groups with different growth patterns using CBCT.
Materials and Methods
Study setting
This retrospective computed tomography (CBCT) study was single-centered and carried out at Saveetha Dental College in Chennai, India from March to April of 2022. Prior to the study commencing, approval was received from the Institutional Human Ethical Committee in February 2022 and accompanied with the clearance number - IHEC/SDC/ORTHO-2105/22/118. Following the guidelines established by the Helsinki Declaration, we obtained written informed consent from each participant before using their CBCT scans for research. The Declaration of Helsinki served as the basis for the entire study's design, which prohibited scanning any patient for research purposes alone.
Sample size
G*Power tool (version 3.0.10., Heinrich Heine University, Düsseldorf) was used to calculate the sample size according to a study conducted by Mahfoud et al.[12] The sample size was estimated to be 90 when calculated with the power being 80% and the alpha level as 0.05. The study consisted of subjects for whom CBCT was taken for diagnostic purposes. Data was gathered from the Department of Oral and Maxillofacial Radiology, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Chennai.
Sample selection
All acquired CBCTs were screened for eligibility. Inclusion criteria for the samples involved patients of pre adolescence (0-12y), adolescence (13-20y), and adulthood (21-35y), of any gender, having skeletal class l relationships. Syndromic patients and those with craniofacial anomalies, systemic diseases, facial asymmetry, congenitally missing, extracted or supernumerary lower incisors, impacted lower anteriors, history of head or dental injuries, orthodontic or orthognathic treatment and endodontic or periodontal diseases were excluded. The eligible CBCT samples were then categorised into subgroups based on their growth pattern.
CBCT
CBCT of the skull for each subject was standardized with an FOV of 8/5mm, tube current of 4mA, 120 kVp peak voltage, 15 seconds exposure time, and a radiation dosage of 496 mGy.cm2. All subjects were standing, and positioned in their natural head position using the canthomeatal orientation line. The Frankfort horizontal plane was oriented parallel to the floor with the midsagittal plane perpendicular to it. The subjects were told not to swallow, their teeth were placed in their maximum intercuspation, and their tongue was pressed up against their palate. [13]
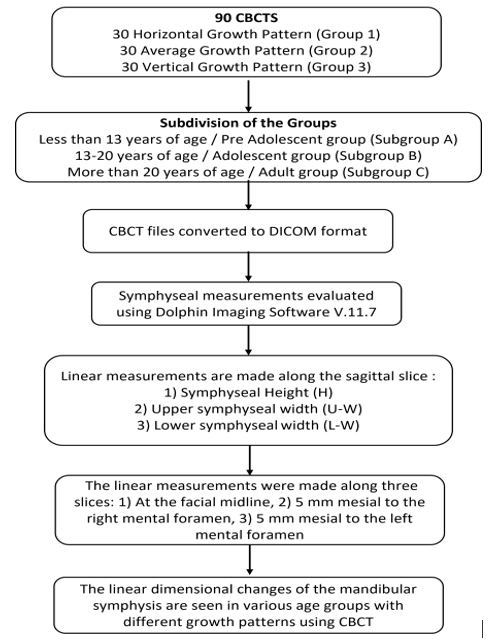
The CBCT scans were generated in DICOM format and assessed using Dolphin Imaging software (Dolphin Imaging and Management Solutions, Patterson Dental Holdings, version 11.85). The age of the patients was marked and basal plane angle was measured. The workflow representation of the steps involved in the methodology is depicted in [Figure 1].
Orientation of the CBCT
The CBCTs were oriented in natural head position using extra oral photographs as reference and verified along the mid sagittal, transverse, and vertical planes using Dolphin 3D Imaging Software.
The samples were divided into 3 groups based on the growth pattern:
The basal plane angle values were calculated as on Rakosi’s cephalometric analysis.
The samples were additionally categorized into age-based subgroups such as Group A aged less than 13 years - Pre-adolescent group (1A - HGP, 2A - AGP, 3A - VGP), Group B aged between 13 to 20 years - Adolescent age group (1B - HGP, 2B - AGP, 3B - VGP) and Group C aged more than 20 years - Adult age group (1C - HGP, 2C - AGP, 3C - VGP). Each subgroup consisted of 10 CBCT samples each.
Measurements
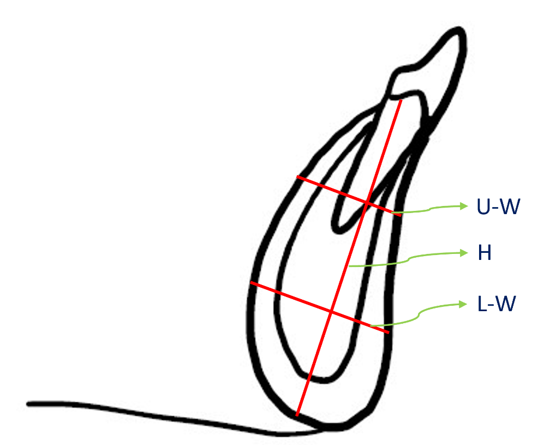
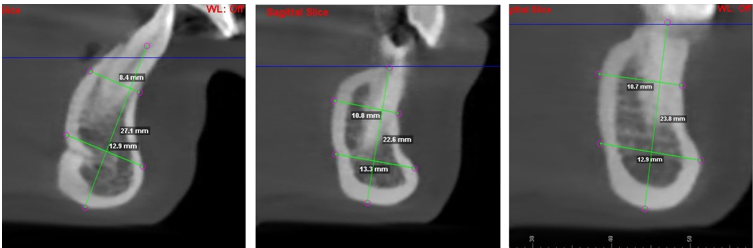
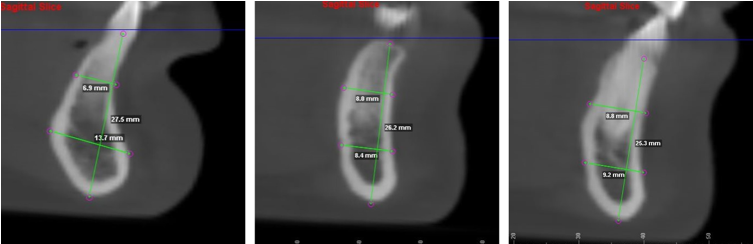
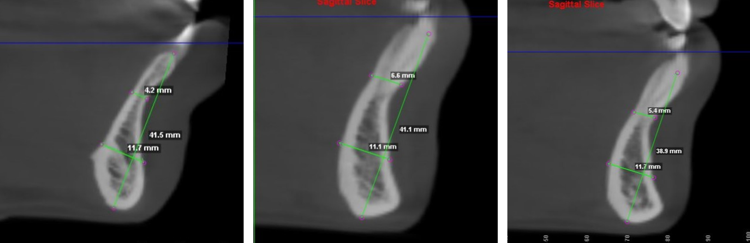
All the linear measurements of the symphyseal region were made in the sagittal slice at the most convex point. The symphyseal height (SH) was determined by measuring the longest distance between the alveolar crest’s highest point and the mandibular inferior border’s lowest point. The symphysis was further divided vertically. The upper width (U-W) was measured as the distance between labial and lingual outer cortices at the intersection of the upper and middle thirds of the symphysis, which is perpendicular to the symphyseal height as stated previously. The lower width (L-W) was measured as the distance between labial and lingual outer cortices at the intersection of the middle and lower thirds of the mandible, perpendicular to the symphyseal height. ([Figure 2])
[Figure 2]: Linear measurements of the mandibular symphysis
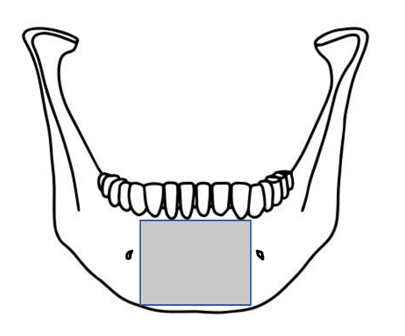
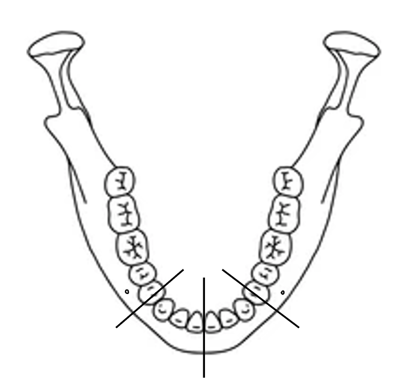
Research conducted by Altug et al. illustrated that the symphyseal borders extended 5 mm anterior to the mental foramen.[14] Therefore, the linear measurements were made along three slices: 1) At the facial midline, 2) 5 mm mesial to the right mental foramen 3) 5 mm mesial to the left mental foramen. [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7]
|
Groups |
Landmark |
Mean ± S.D (mm) |
|
HGP |
SH Midline |
28.547 ± 2.7782 |
|
SH Right |
28.087 ± 3.0670 |
|
|
SH Left |
28.040 ± 3.0582 |
|
|
U-W Midline |
8.120 ± 1.2541 |
|
|
U-W Right |
9.407 ± 1.8116 |
|
|
U-W Left |
9.400 ± 1.8103 |
|
|
L-W Midline |
12.693 ± 1.8211 |
|
|
L-W Right |
11.140 ± 1.9035 |
|
|
L-W Left |
11.493 ± 2.0522 |
|
|
AGP |
SH Midline |
30.667 ± 4.4207 |
|
SH Right |
29.827 ± 3.9094 |
|
|
SH Left |
29.247 ± 4.2618 |
|
|
U-W Midline |
7.180 ± 1.9423 |
|
|
U-W Right |
8.627 ± 1.8460 |
|
|
U-W Left |
8.720 ± 1.6886 |
|
|
L-W Midline |
12.433 ± 1.6666 |
|
|
L-W Right |
9.960 ± 2.4899 |
|
|
L-W Left |
10.053 ± 2.6796 |
|
|
VGP |
SH Midline |
34.207 ± 4.5054 |
|
SH Right |
32.360 ± 4.1304 |
|
|
SH Left |
32.160 ± 4.3217 |
|
|
U-W Midline |
6.013 ± 1.6633 |
|
|
U-W Right |
7.740 ± 1.2955 |
|
|
U-W Left |
7.707 ± 1.7767 |
|
|
L-W Midline |
11.373 ± 2.2811 |
|
|
L-W Right |
10.327 ± 2.0780 |
|
|
L-W Left |
10.267 ± 2.0160 |
|
SH Right |
A |
1 |
1.039 |
.368 |
|
2 |
||||
|
3 |
||||
|
1 |
14.075 |
.000 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
4.177 |
.026 |
|
|
2 |
||||
|
3 |
||||
|
SH Left |
A |
1 |
0.289 |
.752 |
|
2 |
||||
|
3 |
||||
|
1 |
19.904 |
.000 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
5.116 |
.013 |
|
|
2 |
||||
|
3 |
||||
|
U-W Midline |
A |
1 |
5.356 |
.011 |
|
2 |
||||
|
3 |
||||
|
1 |
4.954 |
.015 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
21.441 |
.000 |
|
|
2 |
||||
|
3 |
||||
|
U-W Right |
A |
1 |
2.502 |
.101 |
|
2 |
||||
|
3 |
||||
|
1 |
4.276 |
.024 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
7.857 |
.002 |
|
|
2 |
||||
|
3 |
||||
|
U-W Left |
A |
1 |
0.996 |
.382 |
|
2 |
||||
|
3 |
||||
|
1 2 |
3.247 |
.054 |
||
|
3 |
||||
|
C |
1 |
19.127 |
.000 |
|
|
2 |
||||
|
3 |
||||
|
L-W Midline |
A |
1 |
0.197 |
.822 |
|
2 |
||||
|
3 |
||||
|
1 |
1.459 |
.250 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
9.021 |
.001 |
|
|
2 |
||||
|
3 |
||||
|
L-W Right |
A |
1 |
4.801 |
.016 |
|
2 |
||||
|
3 |
||||
|
1 |
3.182 |
.057 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
4.972 |
.015 |
|
|
2 |
||||
|
3 |
||||
|
L-W Left |
A |
1 |
3.299 |
.052 |
|
2 |
||||
|
3 |
||||
|
1 |
2.401 |
.110 |
||
|
2 |
||||
|
3 |
||||
|
C |
1 |
7.473 |
.003 |
|
|
2 |
||||
|
3 |
|
Parameters |
Age Groups |
Coefficient |
Significance |
|
SH Midline |
A |
0.420 |
.000 |
|
|
|||
|
|
C |
||
|
SH Right |
A |
0.350 |
.000 |
|
|
|||
|
|
C |
||
|
SH Left |
A |
0.376 |
.000 |
|
|
|||
|
|
C |
||
|
U-W Midline |
A |
-0.456 |
.000 |
|
|
|||
|
|
C |
||
|
U-W Right |
A |
-0.267 |
.001 |
|
|
|||
|
|
C |
||
|
U-W Left |
A |
-0.314 |
.000 |
|
|
|||
|
|
C |
||
|
L-W Midline |
A |
-0.085 |
.306 |
|
|
|||
|
|
C |
||
|
L-W Right |
A |
-0.169 |
.042 |
|
|
|||
|
|
C |
||
|
L-W Left |
A |
-0.170 |
0.41 |
|
|
|||
|
|
C |
|
Parameters |
Growth Patterns |
Coefficient |
Significance |
|
SH Midline |
1 |
0.409 |
.000 |
|
|
2 |
||
|
|
3 |
||
|
SH Right |
1 |
0.331 |
.000 |
|
|
2 |
||
|
|
3 |
||
|
SH Left |
1 |
0.292 |
.000 |
|
|
2 |
||
|
|
3 |
||
|
U-W Midline |
1 |
-0.358 |
.000 |
|
|
2 |
||
|
|
3 |
||
|
U-W Right |
1 |
-0.293 |
.000 |
|
|
2 |
||
|
|
3 |
||
|
U-W Left |
1 |
-0.288 |
.001 |
|
|
2 |
||
|
|
3 |
||
|
L-W Midline |
1 |
-0.214 |
.010 |
|
|
2 |
||
|
|
3 |
||
|
L-W Right |
1 |
-0.137 |
.100 |
|
|
2 |
||
|
|
3 |
||
|
L-W Left |
1 |
-0.144 |
.083 |
|
|
2 |
||
|
|
3 |
|
|
Pre - adolescent age group (< 13 years) |
Adolescent age group (13-20 years) |
Adult age group (>20 years) |
|
SH |
Significant difference in H at midline. |
Significant difference in H along right and left sides |
No significant difference |
|
U-W |
Significant difference in U-W at midline |
Significant difference in U-W at right and left sides |
No significant difference |
|
L-W |
No significant difference |
No significant difference |
Significant difference in L-W at midline, right and left sides |
Statistical analysis
Statistical tests such as the Q–Q plot and Kolmogorov–Smirnov tests were performed for each group to evaluate the normality of the data. Calculations of the descriptive statistics for each parameter were made based on their growth patterns. To compare the variations in measurements between the separate age groups, one-way analysis of variance (ANOVA) and the Bonferroni post hoc test were employed. The measurements between the right and left sides were differentiated by applying the Independent-t test. Kendall Tau’s b correlation tests were performed to determine the relation between the measured parameters and age as well as the parameters with the growth patterns. IBM SPSS Statistics software (Version 23, Statistical Package for Social Sciences, IBM Corporation) was used for the interpretation of the results using a significance level of P < 0.05.
Results
Kolmogorov-Smirnov and Q-Q Plot tests showed normal distribution of the data. Descriptive statistics were performed to determine the mean and standard deviation of the linear measurements at various landmarks in all three growth patterns. ([Table 1])
One way ANOVA and Bonferroni Post Hoc tests were performed to compare the difference in each measured parameter between the three age groups. ([Table 2]) Significant differences were seen between the landmarks within the assessed age groups. (P < 0.05) Independent sample tests were performed to compare the variations between the right and left sides. No significant difference was seen (P > 0.05). Kendall Tau’s b correlation tests showed a significant correlation between the measured parameter and age ([Table 3]) and the measured parameters and growth patterns ([Table 4]).
Symphyseal height (SH)
Significant differences were seen in SH at the midlines and on the right and left sides in the different growth patterns (P < 0.05). The SH at midline, right, and left borders was increased in VGP when compared with AGP or HGP. The SH at the midline showed a significant difference at a lower age (below 13 years) compared to the SH at the right and left symphyseal borders. The SH at the right and left borders showed an increase in the adolescent age group. There is no change in the adult group.
Upper symphyseal width (U-W)
Significant differences were seen between the U-W at the midlines and on the right and left sides in the different growth patterns (P < 0.05). The U-W was significantly increased in patients with HGP compared to AGP and VGP. The U-W at the midline showed maximum growth below 13 years of age whereas the same at the right and left borders showed an increase in the adolescent age group (between 13-20 years of age).
Lower symphyseal width (L-W)
Significant differences were seen between the L-W at the midlines and on the right and left sides of the three different growth patterns (P < 0.05). Lower width showed a significant difference in the HGP compared to the other growth patterns. The lower symphyseal width showed a delayed growth process and revealed a significant variation only in the adult age group (beyond 20 years of age).
A positive correlation was also seen between age and height. As the age increased, the height of the mandible increased. A weak negative correlation was seen between age and mandibular widths. This indicated that the upper and lower widths of the mandibular symphysis showed no further increase with age.
Discussion
The aim of the current study was to highlight the correlation between the symphyseal morphology (in terms of the linear dimensional changes in height and width) and growth patterns seen in three different age groups. Mandibular symphyseal morphology and various skeletal growth patterns have been linked in previous research, but consideration to age was not given.[15], [16], [17]
Growth pattern
Patients with HGP showed increased U-W and L-W along the midline as well as the lateral borders in all three age groups compared to AGP and VGP. Patients with VGP showed increased SH along the midline as well as the lateral borders in all three age groups compared to AGP and HGP.
Symphyseal height (SH)
The SH along the midline, as well as the right and left borders, were considerably increased in patients having a VGP compared to HGP subjects. The preadolescent age group showed a significant difference in the increase of SH along the midline as compared to the other groups in both growth patterns.
The SH along the right and left borders, however, were increased in the adolescent age group. This shows that the increase in the height of the symphysis at the midline is lesser compared to the lateral segments, as the individual grows. This observation was made in all growth patterns. This is key in planning an adjunct surgical procedure like reduction genioplasty, that addresses an increased lower anterior facial height in hyperdivergent patients. [18], [19]
Upper symphyseal width (U-W)
U-W was significantly increased in patients with HGP. The symphyseal width was reduced in all patients of VGP. This is in accordance with studies by Kohakura et al., Swasty et al., Sadek et al., and Klinge et al. [20], [21], [17], [22] The U-W along the midline showed greater thickness during the preadolescent age. The lateral structures showed more thickness during the adolescent period. This illustrates the sequence of maturity of the symphyseal bone where the midline structures attain maximum thickness, followed by the lateral structures. [23] This is of prime importance in estimating the planned incisor position for treatment. [24] Greater U-W allows for a greater range of inclination correction of the lower anteriors. [25] It could allow for precise planning to prevent dehiscence and fenestrations of the lower anteriors. [26] Thus, the clinical significance of the results of this study is that the compensatory proclination of lower anteriors in skeletal Class II hyperdivergent patients to camouflage for the retrognathic lower jaw should be performed meticulously. Symphyseal morphology must be taken into account when formulating the treatment plan for patients having hyperdivergent patterns.[27], [28], [29]
Lower symphyseal width (L-W)
The L-W showed an increased thickness in HGP patients as well. The L-W is maximum at a later stage in the adult age group. This has clinical implications in the timing of surgical procedures involving genioplasty for correction of the lower facial height. The anteroposterior repositioning of the lower symphysis can preferably be attempted at older age groups, once the complete symphysial growth has been attained.[30]
The age wise differences of the various parameters assessed in the study is tabulated ([Table 5]). The age wise differences followed the same trend in all three growth patterns.
Conventional radiography providing two-dimensional images does not ensure precise results. Thus, with the advent of computed tomography, detailed investigations could be carried out. CBCT has become increasingly popular in orthodontics owing to its lower radiation dose and superior accuracy in surgical treatment planning. [7] This can be further augmented with artificial intelligence AI-based diagnosis and analysis of the CBCTs. [31], [32], [33] Ahn et al., had utilised CBCT images to construct a structural equation modelling (SEM) of the symphyseal morphologies of different growth patterns. [34] Gousman et al., has used CBCT images to evaluate the bone density of different regions of the symphysis by using the Hounsfield Units (HU). [7]
Limitations and Future Prospects
Only a single slice of the maximum cross section of the CBCT was used to measure the dimensional changes, which is not a true representation of a three-dimensional structure. The changes in the contrast and brightness of the Dolphin imaging software could also influence the anatomical borders. The patients were standardized based on age groups, skeletal relationships, and growth patterns. However, gender-based standardization of samples was not attempted. Further standardization of settings while using imaging softwares to make CBCT measurements is required to correlate with other studies conducted similarly for better analysis and understanding. Future studies should include a larger sample size comparing different populations to evaluate regional variations.
Conclusion
The quantitative dimensions of the mandibular symphysis were found to vary with increasing age in different growth patterns. Due considerations are to be given in the preadolescent age group which experiences a significant increase in the SH and the U-W at the midline. The adolescent age group experiences an increase in the SH and U-W on the lateral aspects. Both of these groups did not show any difference in the L-W. In the adult group, there is no distinction in the SH and the U-W. However, an increase in the L-W was seen both at the midline and lateral aspects in the adult group. HGP showed increased U-W and L-W whereas VGP showed increased SH.
A complete CBCT analysis is beneficial to orthodontic treatment planning as the planned incisor position and Holdaway ratio greatly depend on the symphyseal morphology. Meticulous planning is to be taken out for Class ll hyperdivergent cases as their symphyseal dimensions are limited. CBCT analysis of the mandibular symphysis is essential for preoperative surgical planning requiring genioplasty which is advised in older age groups as the lower third develops at a later stage. It is also found to be beneficial for symphyseal graft operations.
Author Contributions
Study conception and design: Srirengalakshmi Muthuswamy Pandian; Data collection, analysis and interpretation of results: Nisshitha Rao Setvaji; Draft manuscript preparation: Nisshitha Rao Setvaji, Srirengalakshmi Muthuswamy Pandian; Revision of manuscript: Srirengalakshmi Muthuswamy Pandian.
Financial Disclosure Statement
The authors declare there are no competing interests to declare.
Source of Funding
Self-funded study
Conflict of Interest
The authors declare no conflicts of interest.
References
- A Björk. Prediction of mandibular growth rotation. Am J Orthod 1969. [Google Scholar]
- RM Beecher. Evolution of the mandibular symphysis in Notharctinae (Adapidae, Primates). Int J Primatol 1983. [Google Scholar]
- Al-Khateeb Sn, Al Maaitah, ES Badran, A Alhaija. Mandibular symphysis morphology and dimensions in different anteroposterior jaw relationships. Angle Orthod 2014. [Google Scholar]
- K Senthil, P Solete. Prevalence of middle mesial canal in the mesial roots of mandibular molar using cone beam computed tomography-an in-vivo radiographic study. Int J Clin Dent 2021. [Google Scholar]
- MS Kumar, K Murugesan, N Hinaz. Surgical treatment modalities in the management of temporomandibular joint disorders. Int J Dent Oral Sci 2021. [Google Scholar]
- F Çağlayan, MA Sümbüllü, HM Akgül, O Altun. Morphometric and morphologic evaluation of the mental foramen in relation to age and sex: an anatomic cone beam computed tomography study. J Craniofac Surg 2014. [Google Scholar]
- J Gousman, JH Park, JM Chae. Evaluating mandibular symphysis bone density according to various skeletal patterns with CBCT. Orthod Craniofac Res 2021. [Google Scholar]
- H Marghalani, G Guan, P Hyun, S Tabbaa, AI Linjawi, Al-Jewair, . Relationship between mandibular symphysis dimensions and skeletal pattern in adults. Folia Morphol 2022. [Google Scholar]
- H Chen, Z Liu, X Hu, B Wu, Y Gu. Comparison of mandibular cross-sectional morphology between Class I and Class II subjects with different vertical patterns: based on CBCT images and statistical shape analysis. BMC Oral Health 2021. [Google Scholar]
- A I Linjawi, AR Afify, HA Baeshen, D Birkhed, KH Zawawi. Mandibular symphysis dimensions in different sagittal and vertical skeletal relationships. Saudi J Biol Sci 2021. [Google Scholar]
- Sella Tunis, T Hershkovitz, I May, H Vardimon, A D Sarig, R Shpack, N. Variation in Chin and Mandibular Symphysis Size and Shape in Males and Females: A CT-Based Study. Int J Environ Res Public Health 2020. [Google Scholar]
- M Mahfoud, H Hassan. Symphysis Morphology And Dimensions In Different Vertical Facial Patterns (Cbct Scan Study). Roman J Stomatol 2015. [Google Scholar]
- LV Claudino, CT Mattos, O Ruellas Ac De, EF Anna. Pharyngeal airway characterization in adolescents related to facial skeletal pattern: a preliminary study. Am J Orthod Dentofac Orthop 2013. [Google Scholar]
- H A Altug, A T Coskun, K Kamburoglu, T Zerener, O Gulen, M Sencimen. . Volumetric Evaluation of Safe Zone for Bone Harvesting From Symphysis Region by Using Cone Beam Computed Tomography. Implant Dent 2016. [Google Scholar]
- M Moshfeghi, M Nouri, S Mirbeigi, A Baghban. Correlation between symphyseal morphology and mandibular growth. Dent Res J 2014. [Google Scholar]
- T Aki, RS Nanda, F Currier, G Nanda. Assessment of symphysis morphology as a predictor of the direction of mandibular growth. Am J Orthod Dentofac Orthop 1994. [Google Scholar]
- MM Sadek, NE Sabet, IT Hassan. Alveolar bone mapping in subjects with different vertical facial dimensions. Eur J Orthod 2015. [Google Scholar]
- JC Posnick. Aesthetic Alteration of the Chin. . Orthognathic Surg 2014. [Google Scholar]
- S Chamberland, WR Proffit, PE Chamberland. Functional genioplasty in growing patients. Angle Orthod 2015. [Google Scholar]
- S Kohakura, K Kasai, I Ohno, E Kanazawa. Relationship between maxillofacial morphology and morphological characteristics of vertical sections of the mandible obtained by CT scanning. J Nihon Univ Sch Dent 1997. [Google Scholar]
- D Swasty, J Lee, JC Huang, K Maki, SA Gansky, D Hatcher. Cross-sectional human mandibular morphology as assessed in vivo by cone-beam computed tomography in patients with different vertical facial dimensions. Am J Orthod Dentofac Orthop 2011. [Google Scholar]
- A Klinge, K Becktor, C Lindh, JP Becktor. Craniofacial height in relation to cross-sectional maxillary and mandibular morphology. Prog Orthod 2017. [Google Scholar]
- P Foosiri, K Mahatumarat, S Panmekiate. Relationship between mandibular symphysis dimensions and mandibular anterior alveolar bone thickness as assessed with cone-beam computed tomography. Dental Press J Orthod 2018. [Google Scholar]
- C Gütermann, T Peltomäki, G Markic, M Hänggi, M Schätzle, L Signorelli. The inclination of mandibular incisors revisited. Angle Orthod 2014. [Google Scholar]
- Q Yu, X G Pan, G P Ji, G Shen. The association between lower incisal inclination and morphology of the supporting alveolar bone--a cone-beam CT study. Int J Oral Sci 2009. [Google Scholar]
- A Gracco, L Luca, MC Bongiorno, G Siciliani. Computed tomography evaluation of mandibular incisor bony support in untreated patients. Am J Orthod Dentofac Orthop 2010. [Google Scholar]
- R Mangla, V Dua, M Khanna, N Singh, P Padmanabhan. Evaluation of mandibular morphology in different facial types. Contemp Clin Dent 2011. [Google Scholar]
- S M Adel, AA Alwafi, SM Pandian, Y M Bichu, LW Abuljadayel, RA Alansari. What are orthodontic residents perusing on social media? A cross-sectional survey. Semin Orthod 2023. [Google Scholar]
- S M Pandian, NH Gandedkar, K Palani, S Kim, YJ Adel, . An integrated 3D-driven protocol for surgery first orthognathic approach (SFOA) using virtual surgical planning (VSP). Semin Orthod. Semin Orthod 2022. [Google Scholar]
- OS Hama Amin, S W Abdulrahman, A Altom, BA Hasan, RH Khdhir, RH Zorab. Facial deformity correction and genioplasty; a case report and literature review. Ann Med Surg 2022. [Google Scholar]
- NR Vaid. Artificial Intelligence (AI) driven orthodontic care: A quest toward utopia. Semin Orthod 2021. [Google Scholar]
- V Katyal, N Vaid. Virtual-First: A virtual workflow for new patient consultation, engagement and education in orthodontics. Semin Orthod 2023. [Google Scholar]
- D Al-Moghrabi, MT Cobourne, P S Fleming. Orthodontics in the era of social media: An interview with orthodontic journal editors. Seminars Orthod 2023. [Google Scholar]
- MS Ahn, SM Shin, T Yamaguchi, K Maki, TJ Wu, CC Ko. Relationship between the maxillofacial skeletal pattern and the morphology of the mandibular symphysis: Structural equation modeling. Korean J Orthod 2019. [Google Scholar]
