- Visibility 44 Views
- Downloads 17 Downloads
- DOI 10.18231/j.jco.2022.031
-
CrossMark
- Citation
Effect of rapid maxillary expander with posterior bite blocks in hyperdivergent patients with adenoid hypertrophy- A cephalometric study
Introduction
Adenoids, a mass of lymphoid tissue in the nasopharyngeal mucous membrane, are located posterior and superior to the soft palate corresponding to the basal aspect of the sphenoid bone.[1] Scammon’s classic growth curve, demonstrates a rapid rise in infancy and early childhood in the normal growth and size of tonsils and Adenoids, then a slow growth during late childhood and pre puberty, finally regressing gradually to adult size.[2]
Adenoid hypertrophy is one of the few common pathologies causing upper airway obstruction, in turn affecting maxillofacial and dental development in children with active growth. Enlargement of adenoids causes occlusion of the posterior nasal aperture called Choana during sleep in supine position. General features of nasopharyngeal obstruction are mouth breathing, insufficient nasal resonance during speech and snoring and other serious conditions like Otitis media, conductive hearing loss, Obstructive sleep apnea, retardation of growth and pulmonary cardiovascular disease causing right sided heart failure.[3], [4], [5]
Adenoid facies[6] are characterized by long, open mouthed face with an incompetent lip seal, flat nose, small and underdeveloped nostrils, increased lip separation, short and hypotonic upper lip and hypertrophic and everted lower lip, a constricted maxillary arch, retroclined lower incisors, steep mandibular plane angle, large anterior face height, retrognathic mandible, excessive eruption of the molars due to inadequate surface contact, mandible rotation in a downward and backward direction, open bite and unilateral or bilateral posterior cross bite due to insufficient maxillary lateral expansion.[7]
Rapid maxillary expansion (RME) is an orthopaedic procedure for treating transverse maxillary deficiency, first reported by Angell[8] in 1860 and brought into vogue by Haas[9] a century later. It was hypothesized that with maxillary arch expansion, girth and capacity of nasal cavity also increases.[10] As maxillary bones form fifty percent of the nasal cavity’s architecture , RME causing opening of midpalatal suture also leads to outward displacement of nasal cavity’s lateral walls, thus increasing the volume and decreasing nasal airway resistance.[11] The bonded rapid maxillary expansion with occlusal envelope on posterior teeth, allows minimal maxillary molar extrusion and tipping as the occlusal forces are guided against the acrylic, therefore reducing the mandibular rotation in downward and backward trajectory. Bonded RME implicates intrusion on maxillary first molars, therefore contributes to the maintenance of the lower facial height and minimizes the risk of bite opening inevitable with RME.[12] The objective of this study was to cephalometrically evaluate the effect of RME with occlusal bite blocks on posterior teeth, on the dimensions of craniofacial structures forming naspharyngeal airway and related tissues in adenoid hypertrophy patients and to compare them with controls. Rationally if RME increases pharyngeal airway dimensions and improves the sagittal relation between jaws then it can be an important treatment modality for patients suffering from airway obstruction. It may also diminish the need for invasive surgical intervention for airway obstruction at a later date.
Materials and Methods
This study was presented for conduction in the Department of Orthodontics and Dentofacial Orthopaedics in collaboration with Department of Otolaryngology. The randomized clinical trial received ethical approval for execution from Institutional panel for scientific ethics. Written informed consent from parents/guardian was obtained prior to the start of study.
Criteria for selection of subjects
Untreated patients with adenoid hypertrophy were selected with following criteria:
Inclusion criteria
Presence of adenoid hypertrophy as diagnosed by an Otolaryngologist.
Age group between 8-12 years.
Exclusion criteria
No antecedent history of any orthodontic procedure.
No history of upper airway surgeries before or during treatment.
No history of any other Respiratory diseases, history of facial trauma or medical condition that might alter growth.
For this prospective study, a sample of 32 adenoid hypertrophic patients (7 females and 25 males) were selected. The patients were randomly assigned into two groups by the envelope draw method. Each time a new patient arrived, an envelope was picked arbitrarily from 32 envelopes prepared for the purpose. Two groups were categorized among the patients, Group A: (n=16) RME with posterior bite block group and Group B: (n=16) Control group. In Group A, Lateral cephalograms and Posteroanterior cephalograms were recorded before initiation of Treatment (T0), Immediately post expansion; i.e. when the buccal cusps of the mandibular molars were bestrided upon by the palatal cusps of the maxillary molars (T1), and succeeding 9 months of retention (T2). In Group B same radiographs were recorded at the beginning (T0), and after 9 months (T2) in concurrence with Group A. These radiographs were compared for skeletal, dental and soft tissue changes in craniofacial structures in three dimensions.
Design of the rapid maxillary expansion appliance with posterior bite blocks.
|
Variable |
Group A |
Group B |
||||
|
T0 (Mean±SD) |
T1 (Mean±SD) |
T2 (Mean±SD) |
T0 (Mean±SD) |
T2 (Mean±SD) |
||
|
Lateral cephalometric measurements |
||||||
|
1. |
SNA (o) |
76.75±3.941 |
77.38±4.048 |
77.75±4.008 |
78.56±3.464 |
79.06±3.454 |
|
2. |
SNB (o) |
73.94±2.380 |
73±3.120 |
73.81±3.637 |
75.06±3.065 |
74.67±3.005 |
|
3. |
ANB (o) |
2.81±2.344 |
4.50±2.477 |
4.56±2.529 |
3.50±2.422 |
5.19±2.536 |
|
4. |
SN MP(°) |
35.31±3.754 |
36.38±3.594 |
35.13±4.113 |
31.13±3.631 |
32.81±3.936 |
|
5. |
MxI-NA(°) |
28.75±7.506 |
29.38±6.791 |
28.50±6.812 |
18.75±6.486 |
20.56±7.72 |
|
6. |
A-NPerp(mm) |
-1.969±4.316 |
-.50±4.305 |
-.75±3.821 |
-.313±3.198 |
-1.13±3.879 |
|
7. |
Pog-NPerp (mm) |
-8.531±3.658 |
-10.1±3.793 |
-10.7±5.053 |
-5.438±3.326 |
-6.81± 3.449 |
|
8. |
ANS-Me (%) |
57.32±2.723 |
56.46±2.814 |
56.44±2.849 |
54.56±2.809 |
54.80±2.612 |
|
9. |
Zarabak ratio (%) |
62.98±4.442 |
62.65±3.690 |
61.76±3.523 |
64.85±4.301 |
64.55±4.742 |
|
10. |
Soft tissue facial angle(°) |
88.38±2.729 |
88.94±3.785 |
89.75±3.679 |
90.25±2.352 |
89.69±2.469 |
|
PA cephalometric measurements |
||||||
|
1. |
Mo-Mo(mm) |
22.69±1.448 |
22.88±1.360 |
23.25±1.528 |
21.06±2.205 |
23.25±2.082 |
|
2. |
Ln-Ln(mm) |
27.31±1.401 |
28.75±1.571 |
29.06±1.436 |
26.44±2.308 |
29.06±2.366 |
|
3. |
Zyg-Zyg(mm) |
110.31±4.143 |
111.75±3.924 |
112.69±3.737 |
100.69±4.799 |
101.69±4.965 |
|
4. |
J-J (mm) |
60.19±3.970 |
61.81±3.655 |
61.94±3.623 |
58.25±4.282 |
58.94±4.266 |
|
5. |
U6R-U6L (mm) |
53.81±3.038 |
57.44±2.898 |
57.06±2.955 |
52.38±4.048 |
53.06±3.898 |
|
S.N |
Variable |
Group A |
Group B |
||||||
|
|
|
T0-T1 Mean Difference +SD |
P Value |
T1-T2 Mean Difference+SD |
P Value |
Mean Difference +SD |
P Value |
T0-T2 Mean Difference +SD |
P Value |
|
Lateral cephalometric measurements |
|||||||||
|
1. |
SNA (o) |
-.625±1.147 |
.046* |
-.375±1.20 |
0.232 |
-1.000±1.21 |
.005** |
.500±.632 |
0.06 |
|
2. |
SNB (o) |
.938±1.769 |
.051 |
-.813±1.37 |
.032* |
.125±1.708 |
.774 |
.625±.806 |
.007** |
|
3. |
ANB (o) |
-1.68±1.702 |
.001** |
-.063±1.52 |
.872 |
-1.750±1.65 |
.001** |
-.313±.602 |
.05 |
|
4. |
SN MP(°) |
-1.06±1.289 |
.005** |
1.250±1.80 |
.014* |
.500±1.265 |
.135 |
-1.68±1.601 |
.036 * |
|
5. |
MxI-NA(°) |
.0625±5.414 |
.651 |
.875±4.50 |
.449 |
1.218±1.19 |
.001** |
-.813±1.328 |
.027* |
|
6. |
A-NPerp(mm) |
1.468±1.687 |
.003** |
.250±1.238 |
.432 |
-1.218±2.10 |
.035* |
-.300±1.782 |
.511 |
|
7. |
Pog-NPerp (mm) |
1.593±4.136 |
.144 |
.625±3.897 |
.531 |
-.00±2.129 |
1.00 |
-.375±1.360 |
.287 |
|
8. |
ANS-Me (%) |
.8625±1.784 |
.072 |
.0188±1.67 |
.965 |
.938±1.482 |
.023* |
-.250±1.000 |
.333 |
|
9. |
Zarabak ratio (%) |
.3312±1.350 |
.342 |
.8874±1.65 |
.049* |
1.438±3.61 |
.035* |
1.875±5.40 |
.185 |
|
10. |
Soft tissue facial angle(°) |
-.563±3.265 |
.501 |
1.188±3.46 |
.041* |
-.625±2.94 |
.409 |
.563±2.308 |
.345 |
|
|
PA Cephalometric measurements |
||||||||
|
1. |
Mo-Mo(mm) |
-.188±.403 |
.083 |
-.375±.50 |
.009** |
-.563±.512 |
.001** |
-.188±.403 |
.083 |
|
2. |
Ln-Ln(mm) |
-1.438±.629 |
0.0*** |
-.313±.873 |
.173 |
-1.750±1.12 |
0.0*** |
-.563±2.308 |
.345 |
|
3. |
Zyg-Zyg(mm) |
-1.438±1.45 |
.001** |
-.938±1.56 |
.030* |
-2.375±2.63 |
.003** |
-.5688±.793 |
.253 |
|
4. |
J-J (mm) |
-1.625±.885 |
.000*** |
-.125±.719 |
.497 |
-1.750±.931 |
0.0*** |
-.688±.602 |
0.430 |
|
5. |
U6R-U6L (mm) |
-3.625±1.89 |
0.0*** |
.375±.719 |
.054 |
-3.250±1.65 |
0.0*** |
-1.188±.834 |
0.196 |
|
S. No. |
Variable |
T0-T2 of Group A Mean Difference +SD |
T0-T2 of Group B Mean Difference +SD |
Mean Difference Between Group A and Group B |
Un-Paired t |
P Value |
|
|
|
|||||
|
Lateral cephalometric measurements |
||||||
|
1. |
SNA (o) |
-1.000±1.21 |
-.500±.632 |
-.50 + .578 |
1.46 |
0.15 |
|
2. |
SNB (o) |
.125±1.708 |
.625±.806 |
-.500+ .902 |
1.05 |
0.29 |
|
3. |
ANB (o) |
-1.750±1.65 |
-.313±.602 |
-1.437+. 048 |
3.27 |
0.002** |
|
4. |
SN MP(°) |
.500±1.265 |
-1.68±1.601 |
2.18+ .336 |
4.27 |
0.0001*** |
|
5. |
MxI-NA(°) |
1.218±1.19 |
-.813±1.328 |
2.031+ . 138 |
4.55 |
0.0008*** |
|
6. |
A-NPerp(mm) |
1.218±2.10 |
-.300±1.782 |
1.518±.318 |
2.19 |
0.03* |
|
7. |
Pog-NPerp (mm) |
.00±2.129 |
-.375±1.360 |
.375±.859 |
0.59 |
0.55 |
|
8. |
ANS-Me (%) |
.938±1.482 |
-.250±1.000 |
1.188±.482 |
2.66 |
0.012* |
|
9. |
Zarabak ratio (%) |
1.438±3.61 |
1.875±5.40 |
-.437±1.79 |
0.27 |
0.79 |
|
10. |
Soft tissue facial angle(°) |
-.625±2.941 |
.563±2.308 |
-1.188±.633 |
1.27 |
0.21 |
|
PA cephalometric measurements |
||||||
|
1. |
Mo-Mo(mm) |
-.563±.512 |
-.188±.403 |
-.375±.109 |
2.17 |
0.04* |
|
2. |
Ln-Ln(mm) |
-1.750±1.125 |
-.563±2.308 |
-1.187±1.183 |
1.85 |
0.04* |
|
3. |
Zyg-Zyg(mm) |
-2.375±2.630 |
-.5688±.793 |
-1.807±1.837 |
2.69 |
0.01* |
|
4. |
J-J (mm) |
-1.750±.931 |
-.688±.602 |
-1.062±.329 |
1.83 |
0.0006*** |
|
5. |
U6R-U6L (mm) |
-3.250±1.653 |
-1.188±.834 |
-2.062±.819 |
4.45 |
0.0001*** |

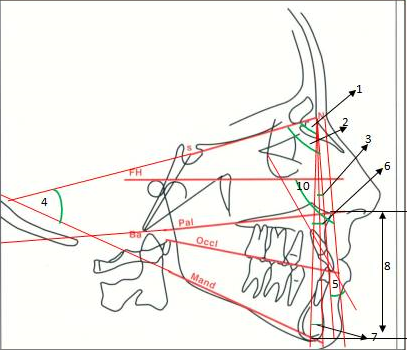
Appliance was constructed by incorporating a hyrax screw into a scaffolding made from .040 inch stainless steel wire. The wire enveloped the teeth starting from the buccal aspect of maxillary first molar corresponding to the mesiobuccal cusp, continuing anteriorly then crossed the occlusion between maxillary deciduous canines and first premolar or deciduous first molars to the lingual surfaces of the teeth, and reaching out posteriorly behind the maxillary first permanent molars. The screw was adapted to the palate with the midline coinciding with the mid palatal suture, 2mm farther from the palate. 2 to 3 mm of cold cure acrylic was introduced on to the maxillary posterior teeth to augment the occlusal bite ([Figure 1]).
Expansion and retention schedule
The appliance was set into motion with one fourth turn two times a day until pertinent amount of expansion was noted i.e. the palatal cusps of the maxillary molars bestrided the buccal cusps of the mandibular molars. After achieving the essential statutory expansion, the RME screw was secured in position with cold cure acrylic and left there as retention appliance for an additional nine months to allow for adequate re-ossification of the maxillofacial sutures disintegrated in the process. Oral hygiene of the patients was maintained throughout the treatment.
Statistical Analysis
Pre-treatment, post-expansion and post-retention Lateral and PA cephalometric values were measured and their significance were compared using the standardized student ‘t’ test. Paired -t test assessed the difference in the amount of change in the different variables between the pre-treatment (T0), post-expansion (T1) and post-retention (T2) in Group A and unpaired -t test compared the changes in Group A with Group B. Significance was determined as *significant at p< 0.05), **highly significant at p< 0.01 and ***very highly significant at p<0.001 levels of confidence. Statistical analysis was conducted using EPI INFO STATISTICS (version 7.0).
Results
Statistically significant findings were as follows:
On lateral cephalogram, in treatment group angle SNA was increased by -1.000±1.21 and ANB was increased by 1.68±1.702 which was statistically highly significant (P< 0.01). It was not statistically significant in control group. SN-MP angle was decreased by .500±1.265 which was not significant (p > 0.05) in Group A but opposite and contrast happened in Group B where there was a statistically significant increase in this angle (p< 0.05). ([Table 2])
In Group A there was a highly significant decrease in MxI-NA° of 1.218±1.19 (P<0.01) it increased significantly in Group B (p< 0.05). The distance point A-NPerp increased significantly in Group A by -1.218±2.10 (p< 0.05) while in Group B there wasn’t any significant change. The distance Pog- NPerp was not changed significantly in both the categories ([Table 2]).
The lower anterior facial height and jarabak’s ratio decreased significantly in Group A by .938±1.482 and 1.438±3.61 respectively(p< 0.05).These values were not changed significantly in Group B(p > 0.05) The changes in soft tissue parameters i.e soft tissue facial angle were statistically insignificant in both the groups(p > 0.05).
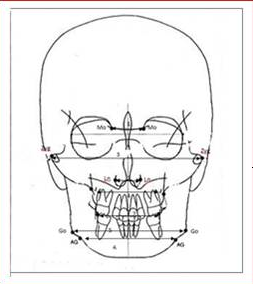
On PA cephalogram all the maxillary transverse parameters were increased significantly in Group A (p< 0.05) while the changes were insignificant in Group B (p > 0.05). In Group A, Mo-Mo increased significantly by -.563±.512 (p<0.05). Increase in Ln-Ln by -1.750±1.125 was highly significant (P<0.01 ). Zyg- Zyg increased by -2.375±2.630 (p< 0.05) and J-J increased by -1.750±.931 (p< 0.05). The increase in U6R-U6L by -3.250±1.653 was highly significant (P<0.01). ([Table 2])
The difference in changes from T0-T2 in Group A in comparison to Group B was statistically highly significant in case of angle ANB°( -1.437+. 048) (P<0.01) and very highly significant in SN-MP°(2.18+ .336 )(p< .001), very highly significant in MxI-NA°(2.031+ . 138 )(p< 0.001), significant in case of point A –Nperp (1.518±.318) (p< 0.05),and significant in case of lower facial height(1.188±.482) (p< 0.05). On PA cephalogram this difference was significant in case of Mo-Mo(-.375±.109), Ln-Ln-(-1.187±1.183), (Zyg-Zyg-1.807±1.837) (p< 0.05) while highly significant in case of J-J(-1.062±.329) and U6R-U6L(-2.062±.819) (p< 0.001)( [Table 3])
Discussion
Adenoid hypertrophy leading to narrowing of the pharyngeal airway and mouth breathing causes maxillary constriction which in turn is associated with problems like cross bites (dental and/or skeletal), discordance in occlusal relationship, esthetics and functional problems like speech and breathing.[12] Timms [13] reported a 37% diminution in nasal airway recalcitrance on an average with RME. Respiratory symptoms are also rectified at the end of treatment with the institution of nasal breathing and achievement of near normalcy of morphology of craniofacial structures forming the nasopharygeal airway. Cephalometric radiography has been very crucial in diagnosis and treatment planning hitherto. It is an important tool for measuring the Pharyngeal airway dimension and craniofacial morphology. Low cost, convenience and reduced exposure to radiation and the ability to simultaneously analyze head position and craniofacial morphology are its major advantages.
In this study, the overall increase in SNA angle found statistically highly significant (p<0.01)([Table 2]) can be due to downward and forward movement of anterior maxillary segment in the sagittal plane after expansion. This was in accordance with the previous reports of Haas,[9] Davis and Kronman.[14] However our data contradicted the findings of Sarver and Johnston[15] who found a backward maxillary movement consequent to bonded RME therapy. The overall decrease in the SNB angle was statistically not significant(P>0.05)([Table 2]). An overall increase in ANB angle of -1.75±1.6 was seen through out treatment which was highly significant (P<0.01)([Table 2]). The increase in the ANB angle was probably due to downward and forward advancement of the maxillary anterior segment and mandibular rotation in downward and backward direction as supported by previous studies.[10], [11], [12] During the retention period, the increase in the ANB angle was reduced due to positioning of the mandible anteriorly because of expansion. Same thing was experienced by McNamara in his study.[16] In the present study, an overall insignificant (p>0.05) decrease of -.500±1.265°([Table 2]) in SN-MP angle was seen. Previous studies by Davis and Kronman[14] and Wertz [17] showed that mandibular plane angle was increased in the cases treated with banded RME. Sarver and Johnston[15] reported that the mandible was not rotated downward and backward when a bonded RME was used. The decrease in the SN-MP angle seen after retention period in RME group highlights the posterior ‘‘bite block effect’’ of Bonded RME in controlling the increase in vertical height seen commonly with adenoid hypertrophy and banded RME treatment. Intrusion of the maxillary molars was noticeably remarkable in the bonded RME managed by Wendling et al.[18] which might probably resulted in auto-rotation of the mandible in the forward and upward direction. In Group B there was a significant (p<0.05) increase by –1.68±79° ([Table 2]) in SN-MP angle from T0 toT2 depicting continuing vertical growth pattern. There was a statistically highly significant (p<0.01) decrease in the inclination of maxillary incisors shown by MxI -NA° from T0 to T2 ([Table 2]) by -.781±6.354 ([Table 2]) whereas the mandibular incisors proclined. This effect was due to relocation of max. incisors into the space created by expansion. Chung et al. reported Similar findings in their studies.[19] The value of linear distance A-NPerp increased significantly (p<0.05) by -1.218±2.108mm in Group A from T0-T2([Table 2]) implying point A was advanced due to RME treatment.
The value of lower anterior facial height measured in terms of percentile of total facial height depicted by ANS-Me decreased from T0-T2([Table 2]) by .938±1.482% which was statistically significant(p<0.05). These values are similar to the study by Omar Gabriel et al.[20] This effect may be due to bite blocks/ RME. In controls, there a statistically insignificant (P>0.05) increase (-.250±1.0%) ([Table 2]) was found attributable to the the possible effect of continued growth changes.
The decrease in Jarabak’s ratio from T0-T2 ([Table 2])in group A by 1.438±3.614 was statistically significant(p<0.05) , was due to the bite block effect of the bonded RME. This decrease by 1.875±5.402 ([Table 2]) in group B, was statistically insignificant (P>0.05)
Soft tissue facial angle, athough increased from T0-T2 ([Table 2]) in group A by -.625±2.941°, was statistically insignificant (P>0.05), and was due to the forward movement of the mandible during the retention phase due to bonded RME. This value decreased by .563±2.308°([Table 2]) in group B , but was statistically insignificant (P>0.05), and was possibly due to continued growth trend.
Lateral rotation with the center on the spheno-occipital synchondrosis or the frontonasal suture separates the maxillary halves in the transverse plane. Since maxillary halves are separated at the first appointment, the forces during the expansion are completely applied to the maxillary bone producing major skeletal effects by RME in mixed dentition. Amount of expansion followed a triangular pattern in our study, with the greatest increase in maxillary arch width (intermolar), followed by the maxillary width (J-J), the nasal width (Ln-Ln), zygomatic width and interorbital width (Mo-Mo). Previous studies by, Haas,[9] Wertz,[17] Chung[19] reported a similar pattern .
In the present study the linear measurements from PA cephalograms were taken to substantiate maxillary expansion in transverse plane. In our study, the mean duration from the pretreatment (T0) to T2 i.e. post retention cephalograms was 9 months. There were appreciable increases in intermolar width, maxillary width, nasal width, and zygomatic width from T0 to T1 and from T0 to T2 which were statistically significant (p<0.05). In group A, Mo-Mo increased significantly by -.563±.512 (p<0.05). Increase in Ln-Ln by -1.750±1.125 was highly significant(P<0.01). Zyg-Zyg increased by -2.375±2.630 (p< 0.05) and J-J increased by -1.750±.931 (p< 0.05). The increase in U6R-U6L by -3.250±1.653 was highly significant (P< 0.01). ([Table 2])
These values though increased in Group B during the 9 months follow up period, were statistically non significant (p>0.05). The expansion produced by RME in this study presented with appreciable amount of skeletal expansion as our sample consisted of actively growing patients as reflected by the observations in both the treatment group as well as control group, but with clinically and statistically significant increases in transverse dimensions in the treatment group as compared to the control group.
Intergroup comparison of Group A and Group B ([Table 3]) shows statistically significant difference in changes from T0-T2 in parameters ANB, SN-MP, MP-PP, MxI-NA, A-NPerp, ANS-Me and all the transverse dimensions with a P value of < 0.05. Increase in J-J and U6R-U6L are very highly significant (p <0.001). The difference in changes from T0-T2 in Group A when compared with Group B was statistically highly significant in case of angle ANB°( -1.437+. 048) (P<0.01) and very highly significant in SN-MP°(2.18+ .336 )(p<. 001), very highly significant in MxI-NA°(2.031+. 138) (p< 0.001), significant in case of point A–Nperp (1.518±.318) (p< 0.05), and significant in case of lower facial height(1.188±.482) (p< 0.05). On PA Cephalogram this difference was significant in case of Mo-Mo (-.375±.109), Ln-Ln (-1.187±1.183), (Zyg-Zyg-1.807±1.837) (p< 0.05) while highly significant in case of J-J (-1.062±.329) and U6R-U6L (-2.062±.819) (p< 0.001)([Table 3])
Hence, Bonded RME with posterior bite block appliance, not only improves the transverse discrepancy and facial esthetics but also increases the pharyngeal airway spaces in patients of adenoid hypertrophy. The increased pharyngeal airway volume and improved sagittal relation between the jaws supports the use of this orthopaedic therapy as an important modality for correction of airway obstruction.
Cephalometry as a diagnostic tool has a major shortcoming i.e. a two dimensional representation of a three dimensional structure which can limit the elaborate and accurate evaluation of any real time entity. Cone beam computed tomography (CBCT) and Magnetic resonance (MR) scans are the latest advancements in the field of radiodiagnosis to provide three dimensional measurements of nasopharyngeal airway, but high expense and exposure to high radiation dose are their drawbacks which are worth mentioning.
Conclusion
Interpretation of the study leads to following inferences:
Bite blocks are effective in reducing mandibular plane angle as indicated by SN-MP angle.
Point A and Pogonion point are anteriorly positioned.
Bonded RME is effective in controlling vertical development as lower facial height was reduced and the Jarabak’ ratio decreased.
Bonded RME treatment effectively increased the transverse dimensions of nasopharyngeal airway.
The results of our study conclude that rapid maxillary expansion is effective treatment for increasing the lateral dimensions and capacity of nasopharyngeal airway and institution of nasal breathing in adenoid hypertrophy patients.
Combined with posterior bite blocks, it helps in reducing the detrimental effects of maxillary expansion such as increase in vertical dimension and open bite. Thus institution of this orthopaedic modality of RME with posterior bite blocks at the right time of growth period can be considered as a viable treatment option.
Source of Funding
No specific grant has been received from any funding agency.
Conflict of Interest
The authors declare no conflicts of interest.
References
- O Oliver. The evil effect of adenoids and tonsils upon the dental arches. Int J Orthod 1918. [Google Scholar]
- RE Scammon, JA Harris, CM Jackson, DG Patterson. . The measurement of man 1930. [Google Scholar]
- JL Paradise, BS Bernard, DK Colborn, JE Janosky. Assessment of adenoidal obstruction in children: clinical signs versus roentgenographic findings. J Paediatr 1998. [Google Scholar]
- RT Brouillette, SK Fernbach, CE Hunt. Obstructive sleep apnea in infants and children. J Pediatr 1982. [Google Scholar]
- PW Flint, BH Haughey, KT Robbins, JR Thomas, JK Niparko, VJ Lund. . Cummings Otolaryngology: Head and Neck Surgery 2016. [Google Scholar]
- N Gupta, D Gupta, S Varshney, R Singh, SS Bist, J Barthwala. Orthodontic treatment after adenoidectomy patients: effect on jaw relations in saggital plane. Indian J Otolaryngol Head & Neck Surg 2009. [Google Scholar]
- RM Rubin. Effects of nasal airway obstruction on facial growth.. Ear Nose Throat J 1987. [Google Scholar]
- DH Angell. Treatment of irregularity of the permanent or adult teeth. Dent Cosmos 1860. [Google Scholar]
- AJ Haas. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod 1961. [Google Scholar]
- C Baratieri, M Alves, M Desouza, AMT Desouza, LC Maia. Does rapid maxillary expansion have long-term effects on airway dimensions and breathing?. Am J Orthod Dentofac Orthop 2011. [Google Scholar]
- CC Piskai, MG Boquiren, A Obreza, MGC Viana, N Oppermann, F Sanchez. Assessment of vertical changes during maxillary expansion using quad helix or bonded rapid maxillary expander. Angle Orthod 2016. [Google Scholar]
- YChang, LJ Koenig, JE Pruszynski, TG Bradley, JA Bosio, D Liu. Dimensional changes of upper airway after rapid maxillary expansion: A prospective cone-beam computed tomography study. Am J Orthod Dentofac Orthop 2013. [Google Scholar]
- DJ Timms. A study of basal movement with rapid maxillary expansion. Am J Orthod Dentofac Orthop 1980. [Google Scholar]
- WM Davis, JH Kronman. Anatomical changes induced by splitting of the midpalatal suture. Angle Orthod 1969. [Google Scholar]
- DM Sarver, MW Johnston. Skeletal changes in vertical and anterior displacement of maxilla with bonded rapid palatal expansion appliances. Am J Orthod Dentofac Orthop 1989. [Google Scholar]
- JA Mcnamara, WL Brudon. . Orthodontic and Orthopedic Treatment in the Mixed Dentition 1993. [Google Scholar]
- RA Wertz. Skeletal and dental changes accompanying rapid palatal suture opening. Am J Orthod Dentofac Orthop 1970. [Google Scholar]
- LK Wendling, JR Jam, L Franchi. A Prospective Study of the Short-term Treatment Effects of the Acrylic-splint Rapid Maxillary Expander Combined with the Lower Schwarz Appliance. Angle Orthod 2005. [Google Scholar]
- CH Chung, B Font. Skeletal and dental changes in sagittal, vertical and transverse dimensions after rapid maxillary expansion. Am J Orthod Dentofac Orthop 2004. [Google Scholar]
- FO Ogds, MCV Boas, LC Fo. Rapid maxillary expansion in primary and mixed dentition: A cephalometric evaluation. Am J Orthod Dentofac Orthop 1991. [Google Scholar]
