- Visibility 92 Views
- Downloads 11 Downloads
- DOI 10.18231/j.jco.2022.033
-
CrossMark
- Citation
Clinical applicability of IZC’s in orthodontics - A review
Introduction
Anchorage control acts as the cornerstone of the orthodontic force system. Anchorage is provided by the teeth that resist the forces of reaction generated by the active components of the appliance. So, any unwanted tooth movement must be controlled; otherwise the underlying malocclusion will worsen during tooth alignment and to overcome this problem, skeletal anchorage has been increasingly popularised into orthodontic treatment. Skeletal anchorage involves headgear, mini-plates, palatal arches or temporary anchorage devices in maxilla which resist undesirable mesial movement of the upper molar teeth but the major disadvantage of TAD when inserted inter-radicularlly (I-R) is root damage, and also the failure rates increases three times compared to the TADS placed at extra radicular sites .i.e. I-R TAD anchorage interferes with the path of tooth movement.[1]
Hence, taking both surgical and biomechanical perspectives into consideration, extra-alveolar (E-A) TADS were introduced which has marked a silver lining to overcome the limitations of existing TADS.
Extra-radicular bone screws include IZC in maxilla and BS in mandible classified under temporary anchorage devices which provide skeletal anchorage.[2]
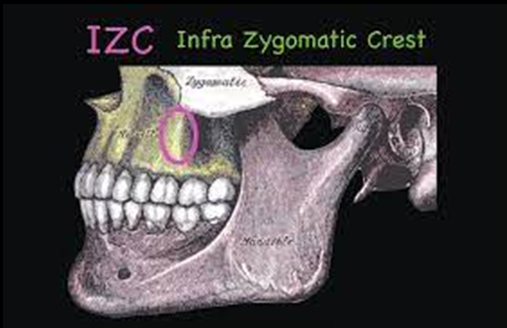
IZC is the stable site at the zygomatic process of maxilla and therefore it is the most preffered site for the placement of EA microimplants. It extends 2cms or more to the zygomaticomaxillary suture- superiorly running lateral to the roots of first and second maxillary molars. Clinically this ridge is palpable along the curvature between the alveolar and zygomatic process of the maxilla however, it varies among young and old individuals and it was found that the crest of the cortical bone is located between maxillary second premolar and first molar in young subjects and above maxillary first molar in adults.[3]
Discussion
Skeletal anchorage has been addressed as a companion to the orthodontic treatment, through which it is possible to correct malocclusions which were either difficult or impossible to be corrected by regular conventional mechanics. Skeletal anchorage devices include micro-implants, mini-plates and dental implants- micro-implants being the most trendy and accepted device among all.[4]
Micro-implants have been effective in bringing tooth movement in all three dimensions of space, whether it is anterior tooth or whole arch retraction, single tooth or whole arch intrusion, molar protraction, canine and premolar distalization with sliding mechanics, asymmetric correction of occlusal plane and midline deviation, as an anchorage for cantilever used for impacted canine traction, orthognathic surgery preparation in class III cases, unilateral distalization, or even bringing about skeletal changes in maxillomandibular relationships while maintaining absolute anchorage.[4], [5], [6], [7]
En-Masse movement of maxillary and mandibular whole dentition was previously only possible by using extraoral forces or orthognathic surgery but now it is possible through the extra radicular micro implants i.e. (IZC in maxilla and buccal shelf in mandible). IZC is the most stable site at the zygomatic process of maxilla hence it is preffered for the placement of extra-alveolar microimplants. ([Figure 1])
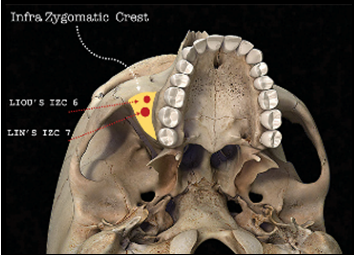
Bone screws are placed on the buccal surface of the alveolar process at the base of the zygomatic crest eminence supporting the roots of the maxillary first and second molars i.e., higher and lateral to the 1st and 2nd molar region but acc. to Lin[8] bone screws to be placed in the 1st and 2nd molar region, while Liou[9] proposed a more anterior placement i.e., closer to the mesiobuccal root of the 1st molar.[10], [11] ([Figure 2])
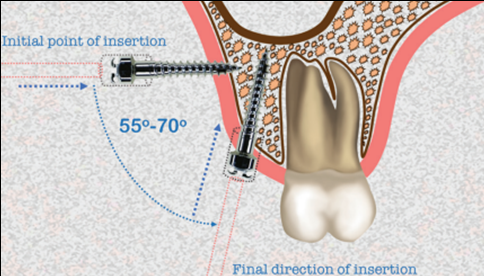
While placing the bone screws the point of insertion is inter-dentally 2 mm above the muco-gingival junction between 1st and the 2nd molar in the alveolar mucosa. The surgical procedure is a two-step process:[10]
The tip of the self-drilling screw is screwed in perpendicular to the axis of the teeth, and
As the screw tip penetrates the cortical plate, the screw driver is rotated 55°–70° towards the tooth (downward) avoiding the roots of the teeth and directing towards the crest area of the maxilla.
According to Liou et al.[9], inserting the miniscrew at an angle of 75o to the maxillary occlusal plane, is technically difficult and the chances of injury to the root and bone stripping is high, contrary to inserting the miniscrew at 40o to the maxillary occlusal plane is technically easy and chances of slippage, damage to the root and bone stripping is less, but the bone depth at this angulation is far less with chances of alveolar or buccal mucosa irritation and to avoid this mucosal irritation they proposed to insert the miniscrew in the keratinized gingiva or the mucogingival junction. Hence, the recommended insertion angle as per the studies is between 55o – 70o.[10] ([Figure 3])
But the failure of changing the angulation at the exact time results in:[12]
Inaccurate ideal final angulation, leading to trauma to the buccal mucosa
Damage to the roots by inter radicular placement of the screw.
To ease the oral hygiene and control over the soft tissue irritation surrounding the head of each bone screw- the screw should be inserted until only the head of the screw is visible outside the alveolar mucosa i.e., it should be placed at the minimum of 5-mm superior to the level of the supporting soft tissue.[13]
Liou et al (2007)[9] reported the clinical implication for miniscrew placement in the infra zygomatic crest in an adult which is 14 to 16 mm above with an insertion angle of 55° to 70° to the maxillary occlusal plane at maxillary first molar whereas with research Lima et al (2021)[14] in his study stated that the most safe zone for IZC miniscrew insertion is between the maxillary first and second molars and on the mesial root of the second molar 11 mm from the alveolar crest in all 3 facial types (hypodivergent, normo-divergent and hyperdivergent).
IZC screws are nothing but a temporary anchorage device therefore, they should hold the basic properties of mini-implant like non-toxicity, low cost with brilliant biocompatibility and mechanical properties and should be stress, strain, and corrosion resistant.[3]
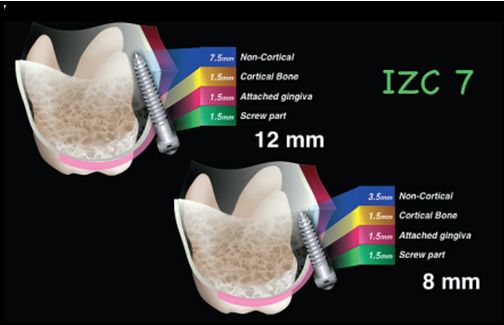
Usually, IZCs exist in two dimensions (manufacturer specific) – 12 and 14 mm in length and a diameter of 2 mm which are larger in dimension compared to mini-implant as an IZC screw penetrates about a 3mm of attached gingiva and cortical bone thickness. The clearance should be ~1.5mm of the screw head to the soft tissue, such that a distance of about 4.5mm exist between the screw base and the inner surface of the cortical bone. Thus, screws of 8-12mm length will extend into the non-cortical bone space (medullary bone or sinus) about 3.5-7.5mm ([Figure 4]) but Ghosh[10] and Chang[13] inferred that the screw head should be at the minimum of 5-mm superior to the level of the supporting soft tissue which compensates for the extension of screw into the sinus which also, helps in maintaining the oral hygiene to prevent irresistible soft tissue inflammation and host factors (pain or root damage) which is problematic for I-R TADs. According to Jia et al (2018)[15] the penetration through double cortical bone plates with limitation of the penetration depth within 1 mm is recommended for infrazygomatic crest mini-implant anchorage.[2], [10], [12], [15]
Among the two sizes of IZC screws i.e., 12 and 14 mm - when the soft tissue in the buccal vestibule is thick the ideal choice is a 14 mm screw (7 mm head + collar area and 7 mm cutting spiral) whereas the screw of 12 mm is an ideal choice in cases where soft tissue is thin in the vestibular region. However, variations exist in the length of cutting spiral, head, and collar dimensions depending on the choice of manufacturer. The shape of the head of screw may also vary, the common being the mushroom shaped and as a short or a long collar depending on the anatomic site and the clinical situation it needs to be used for.[10], [13]
Depending on the material IZCs can be of three types:[3]
Bio tolerant (stainless steel, chromium–cobalt alloy),
Bioinert (titanium, carbon), and
Bioactive (hydroxyapatite, ceramic oxidized aluminium).
Among all Titanium is a suitable material as it does not acquire any immunologic reactions or neoplasm formation and has a property of less fatigue strength and for this reason, an alloy of titanium that is titanium-6 aluminum-4 vanadium is used but the choice of material is pure stainless steel because the bone screws are generally placed in areas of DI (>1250 HU) quality bone (IZC and BS areas) and therefore requires greater fracture resistance, and stainless steel provides greater fracture resistance than Ti alloy and is therefore the preferred material of choice. However, Chang et al (2019)[16] stated that for both IZC and BSS- SS and TiA are clinically acceptable with the success rate of 93.7%.[4], [10], [16]
Once the screw is inserted into the bone, stresses are generated due to the occlusal forces which are transmitted primarily through the infra zygomatic crest chiefly held up by the frontal and temporal processes of the zygomatic bone in different directions. The maximum von mises stress values were seen around the MI, followed by cortical and cancellous bone. However, massive stresses are concentrated onto cortical bone in areas with higher cortical bone density but uniformly distributed to both the cortical and cancellous bone in areas with poor cortical bone density.[17], [18]
Ozdemir et al (2014)[19] proposed that in the anterior region the primary stability of implants is enhanced by increase in cancellous bone density. However, in a present study by Arvind TR. (2021)[18] stated that in the anterior interradicular regions cancellous bone density was maximum and is impervious of the growth patterns. But, on comparing bone density in the posterior regions (buccal and palatal cortical bone) and at the IZC region between low, average and high angle subjects then the low angle subjects have higher density.
Further, Junaid K et al.[20] inferred that von mises stress in alveolar bone (cortical bone) was maximum when IZC was placed at mesiobuccal root of first molar mesialy (107.79 MPa) at the screw fixation site that was within the optimum limit (135 MPa).
Though, clinical success of MI use depends primarily on MI stress transfer to surrounding bone without generating high forces compromising implant stability:[21]
The reduced stress values around MI may lead to bone atrophy.
Elevated stress values in supporting tissues leads to pressure necrosis and subsequent MI failure.
Therefore, long-term success of MI after the healing phase and during the loading phase is primarily dependent on secondary stability and reduced stress in cancellous bone could be a factor that strengthens secondary stability, but because very less attempts are available to evaluate secondary stability therefore, more research is required in that direction.[21]
Paul P. et al.[21] reported that the MI showed maximal von mises stress at 900 and minimal von mises stress at 600 angulations.
As von mises stress is directly proportional to force magnitude- 220 to 340g (8 to 12 oz) of force is required for mechanics with mini-implants in the IZC area but in cases where two step retraction is required i.e., individual retraction of canines and premolars followed by anterior retraction or single tooth retraction then force must be adjusted between 150 and 200 g. So, an optimal force that can be safely loaded onto a micro-implant should not exceed a value of around 3.75–4.5 N as recommended by Alrbata.[6], [22]
However, according to a recent study by Paul P. (2021)[21] both in the MI and the bone maximum and minimum stresses was recorded when load was 12 oz at 8 oz respectively. Hence, the loading force should be between 8 - 12 oz. Therefore, from above wide variations the loading force required for distalization of complete maxillary segment is 300gm to 400gm on each side.[9]
Further, Chopra S[23] and Ghosh A.[10] stated that immediate loading is effective and well tolerated in producing immediate orthodontic anchorage for the retraction i.e., a single bone screw can be immediately loaded with the force of up to 300–350 g.
The pull-out strength and stability of OMIS depend upon the existing thickness and density of the cortical bone and hence, a positive correlation exists between the primary stability and cortical bone thickness.[11], [18]
In regard to the above-mentioned statement primary stability is defined as absence of mobility in the bone bed after miniscrew placement. The factors on which stability is dependent are:[11]
Mechanical engagement of implant with the bone socket.
Bone quality and quantity.
Design and site of implant placement.
Therefore, w.r.t good stability and a high success rate of orthodontic mini-implants >1 mm cortical bone thickness is necessary i.e., the mini-implant should penetrate the double cortical bone plates to obtain adequate primary stability keeping the insertion angle of screw between 50o and 60o in the IZC region.
Moreover, the primary stability of OMIS in sites with deficient cortical bone thickness appears to be influenced by the cortical anchorage provided by bone density.[18]
Acc. to Mavropoulos et al.[24] more than 1 mm of cortical bone thickness is necessary for the stability of the implants but only 1.44 to 1.58 mm is the mean infrazygomatic bone thickness as mentioned by Fransworth.[25] Also, in the study by Chen et al,[26] the mean infrazygomatic (IZ) bone thickness was found to be 5.8 mm, of which more than 6 mm of bone thickness was observed in male group. However, these differences might be due to individual variation in the development of maxillary sinus. Therefore, many studies were conducted using CBCT to measure the mean bone thickness of infrazygomatic crest region.
So, as stated by Liou et al.[9] at 40 and 75-degree insertion angle mean bone thickness was 5.2 mm and 8.8 mm respectively whereas Baumgaertel and Hans[27] observed that the greatest bone depth was at 11.48 mm apical to cementoenamel junction (CEJ) of the maxillary molar. However, with research Murugesan et al.[28] and Amri et al.[29] showed similar results and recommended that at a height of 12 to 17 mm from the occlusal plane with an insertion angle of 65 to 70 degree, 9 to 11 mm implants must be used.[30]
Concerning the present study by Krishnakumaran et al. (2021)[30] the superolateral region of infrazygomatic bone is thickest with the maximum mean bone thickness of 10 mm at zygomatic process of maxilla while the anterior wall of maxillary sinus was thinnest with the maximum mean bone thickness of 5 mm in the completion stage of CVMI i.e., bone density increases with advancing age.
However, for selection of ideal implants precise determination of bone thickness is required due to the close proximity of maxillary sinus and the mesiobuccal root of the maxillary first molar especially in young patients.
As per literature search there are very few studies which have evaluated the IZC bone thickness variations in normo, hypo and hyperdivergent groups. Murugesan et al.[31] proposed that the adequate bone thickness is above the mesiobuccal root of the second molar in all skeletal patterns but in normo and hypodivergent groups it is adequate above the mesiobuccal root of the first molar only. Thus, in hyperdivergent groups it would be desirable to place the IZC screw above the mesiobuccal root of the maxillary second molar.
However, Martias[32] and Vargas[33] showed heterogenous results i.e., no correlation was observed between the bone width in the IZC region and the vertical face height (gonial angle) of the patient and also, proposed that the site buccal to the mesiobuccal root of first molar is best to install miniscrews.
Hence, while concerning above mentioned studies it is always advisable to place the screws in a balanced manner so as to preserve the anatomy and the surrounding structures considering all the factors otherwise the outcomes would be gingival enlargement around the screw, ulceration, early loosening of the screw, maxillary sinus perforation while additional complications that are be associated with the mini-screw are its bending, failure or fracture with the loss in anchorage , but to a lesser extent. Also, when IZC screws are placed asymmetrically on the left and right side of the mouth can lead to alteration of biomechanics.[2], [3], [7]
However, still the controversy exist in the literature regarding the side effects of perforation and therefore, further studies are required.
According to a recent study by Chang et al.[34] failure rate of IZC screw is less than 7% and these failures are due to:
Poor bone quality
Movable mucosa
Low sinus floor
Also, Chang et al.[34] in his study found no significant difference in the failure rate when the screw was placed at least 5mm away from the soft tissue surface i.e. between the movable mucosa and attached gingiva.
Conclusion
Use of IZCs is a very effective therapeutic approach in carefully selected situations as it also aids in treating borderline cases.
IZCs screw should be inserted 2mm above the mucogingival junction (10-12mm above the occlusal plane) on the buccal surface of alveolar mucosa at the base of zygomatic crest eminence supporting the 1st and 2nd molar roots at an insertion angle of 50o – 65o with an immediate load of 8-12 oz. A stainless-steel screw of 12mm in length and 2mm in diameter should be preferred because IZC area is a high density and quality bone area which requires greater fracture resistance and double cortical bone plate penetration for its stability.
However, bone thickness, proximity of anterior wall of maxillary sinus and mesiobuccal root of molars, third molar status, movable mucosa are some of the factors should be taken into consideration during treatment planning.
Source of Funding
None.
Conflict of Interest
None.
References
- CH Chang, LY Lin, WE Roberts. Orthodontic bone screws: A quick update and its promising future. Orthod Craniofac Res 2021. [Google Scholar]
- JJ Lin, WE Roberts. Guided Infra-zygomatic screws: Reliable maxillary arch retraction. Int J Orthod Implantol 2017. [Google Scholar]
- S Sandeep, P Katheesa. An overview of extra alveolar bone screws-IZC/BS screws. Biomedicine 2020. [Google Scholar]
- A Ghosh, A Ray. Posterior maxillary dentoalveolar intrusion with microimplants to avoid the need of a maxillary surgery in the surgical management of skeletal Class III vertical malocclusion. APOS Trends Orthod 2016. [Google Scholar]
- M Kumar, M Goyal, A Kushwah, S Soni. Modified Approach Of Force Application In Izc Mini-Implant For Arch Distalization By Elastomeric Chain. Univ J Dent Sci 2020. [Google Scholar]
- MR Almeida. Biomechanics of extra-alveolar mini-implants. Dental Press J Orthod 2019. [Google Scholar]
- M De Almeida, D Almeida, R Nanda. Biomechanics of extra-alveolar mini-implant use in the infrazygomatic crest area for asymmetrical correction of class II subdivision malocclusion. APOS Trends Orthod 2018. [Google Scholar]
- JJ Lin. A New method of placing orthodontic bone screws in IZC. News Trends Orthod 2009. [Google Scholar]
- EJ Liou, PH Chen, YC Wang, JC Lin. A computed tomographic image study on the thickness of the infrazygomatic crest of the maxilla and its clinical implications for miniscrew insertion. Am J Orthod Dentofac Orthop 2007. [Google Scholar]
- A Ghosh. Infra-zygomatic crest and buccal shelf-Orthodontic bone screws: A leap ahead of micro-implants-Clinical perspectives. J Indian Orthod Soc 2018. [Google Scholar]
- S Pathak, T Patil, A Mahamuni, K Jaju, R Rai. Mandibular buccal shelf and infra zygomatic crest-A safe zone for mini screw insertion. Indian J Orthod Dentofac Res 2019. [Google Scholar]
- S Deshpande, SB Shenoi, R Hattarki. A simple system for improving the accuracy of IZC bone screw placement. APOS Trends Orthod 2020. [Google Scholar]
- CC Chang, JS Lin, HY Yeh. Extra-alveolar bone screws for conservative correction of severe malocclusion without extractions or orthognathic surgery. Curr Osteoporos Rep 2018. [Google Scholar]
- A Lima, RG Domingos, AN Ribeiro, JR Neto, JB De Paiva. Safe sites for orthodontic miniscrew insertion in the infrazygomatic crest area in different facial types: A tomographic study. Am J Orthod Dentofac Orthop 2021. [Google Scholar]
- X Jia, X Chen, X Huang. Influence of orthodontic mini-implant penetration of the maxillary sinus in the infrazygomatic crest region. Am J Orthod Dentofac Orthop 2018. [Google Scholar]
- CH Chang, JS Lin, WE Roberts. Failure rates for stainless steel versus titanium alloy infrazygomatic crest bone screws: A single-center, randomized double-blind clinical trial. Angle Orthod 2019. [Google Scholar]
- K Ujigawa, Y Kato, Y Kizu, M Tonogi, GY Yamane. Three-dimensional finite elemental analysis of zygomatic implants in craniofacial structures. Int J Oral and Maxillofac Surg 2007. [Google Scholar]
- TP Arvind, RK Jain. Computed tomography assessment of maxillary bone density for orthodontic mini-implant placement with respect to vertical growth patterns. J Orthod 2021. [Google Scholar]
- F Ozdemir, M Tozlu, G Cakan. Quantitative evaluation of alveolar cortical bone density in adults with different vertical facial types using cone-beam computed tomography. Korean J Orthod 2014. [Google Scholar]
- J Khan, M Goyal, M Kumar, A Kushwah, A Kaur, M Sharma. Comparative evaluation of displacement and stress distribution pattern during maxillary arch distalization with Infra Zygomatic Screw-A three dimensional finite element study. Int Orthod 2021. [Google Scholar]
- P Paul, AK Mathur, P Chitra. Stress distribution patterns in mini-implant and bone in the infra-zygomatic crest region at different angulations: A finite element study. J World Fed Orthod 2021. [Google Scholar]
- RH Alrbata, MQ Momani, AM Al-Tarawneh, A Ihyasat. Optimal force magnitude loaded to orthodontic microimplants: a finite element analysis. Angle Orthod 2016. [Google Scholar]
- SS Chopra, A Chakranarayan. Clinical evaluation of immediate loading of titanium orthodontic implants. Med J Armed Forces India 2015. [Google Scholar]
- A Mavropoulos, S Kiliaridis, A Bresin, P Ammann. Effect of different masticatory functional and mechanical demands on the structural adaptation of the mandibular alveolar bone in young growing rats. Bone 2004. [Google Scholar]
- D Farnsworth, P Rossouw, E Ceen, RF Buschang. Cortical bone thickness at common miniscrew implant placement sites. Am J Orthod Dentofac Orthop 2011. [Google Scholar]
- YJ Chen, CT Kao. Huang Evaluation of ten extra-alveolar temporary anchorage device insertion sites by cone beam volumetric computer tomography: A pilot study. J Dent Sci 2010. [Google Scholar]
- S Baumgaertel, MG Hans. Assessment of infrazygomatic bone depth for mini-screw insertion. Clin Oral Implants Res 2009. [Google Scholar]
- A Murugesan, A Sivakumar. Comparison of bone thickness in infrazygomatic crest area at various miniscrew insertion angles in Dravidian population-A cone beam computed tomography study. Int Orthod 2020. [Google Scholar]
- Al Amri, MS Sabban, HM Alsaggaf, DH Alsulaimani, FF Al-Turki, GA Al-Zahrani. Anatomical consideration for optimal position of orthodontic miniscrews in the maxilla: a CBCT appraisal. Ann Saudi Med 2020. [Google Scholar]
- M Krishnakumaran, B Krishnan, R Raman, S Rangarajan, G Preethi, A Chinnasamy. Correlation of Infrazygomatic Bone Thickness With Cervical Vertebrae Maturation Stages. J Indian Orthod Soc 2021. [Google Scholar]
- A Murugesan, RK Jain. A 3D comparison of dimension of infrazygomatic crest region in different vertical skeletal patterns: A retrospective study. Int Orthod 2020. [Google Scholar]
- M Matias, CF Mir, MR De Almeida, DA Silva, B Vieira, KM De Freitas. Miniscrew insertion sites of infrazygomatic crest and mandibular buccal shelf in different vertical craniofacial patterns: A cone-beam computed tomography study. Korean J Orthod 2021. [Google Scholar]
- EO Vargas, RL De Lima, LI Nojima. Mandibular buccal shelf and infrazygomatic crest thicknesses in patients with different vertical facial heights. Am J Orthod Dentofac Orthop 2020. [Google Scholar]
- CH Chris, E Hsu, J Lin, HY Yeh, WE Roberts. Comparison of the failure rate for infrazygomatic bone screws placed in movable mucosa or attached gingiva. Eur J Orthod 2017. [Google Scholar]
