- Visibility 55 Views
- Downloads 17 Downloads
- DOI 10.18231/j.jco.2023.021
-
CrossMark
- Citation
Assessment of changes in maxillary dentoalveolar complex following retraction and intrusion of maxillary anterior teeth in mixed Indian population
- Author Details:
-
Pushkar Andhare *
-
Sanjeev Datana
-
Shiv Agarwal
-
SS Chopra
-
ID Roy
Introduction
Alveolar bone is one of the fundamental structures which support dentition. The biology of tooth movement implicates selective resorption and deposition of alveolar bone during orthodontic tooth movement. Therefore, it is expected that the tooth moves along with its dentoalveolar complex to the new position giving rise to the concept of "tooth movement with the bone". Any discrepancy in this pattern of bone resorption and deposition may result in complications such as external root resorption, gingival recession, alveolar bone loss, dehiscence & fenestration as sequela to "tooth movement through the bone".[1]
A large number of patients report to orthodontic clinics for correction of bimaxillary protrusion and for correction of increased overjet & overbite.[2] Therefore, the most commonly required orthodontic tooth movement would be retraction and intrusion of anterior teeth. Moreover, it is during this type of orthodontic tooth movement that maximum modelling and remodelling of dentoalveolar housing tend to occur. Hence, it is essential to understand this change in dentoalveolar housing, so as to avoid iatrogenic effects and obtain a stable treatment outcome.[1]
The cortices of the alveolar bone are considered boundaries of the alveolar complex that limit the orthodontic tooth movement and act as an "Orthodontic Wall" for movement of teeth.[3] It is the thickness of bone available between these cortices and the roots of teeth, which determines the possible extent of orthodontic tooth movement. Therefore, it is pertinent to determine the thickness of bone available, before planning any orthodontic tooth movement. With the advent of latest three-dimensional (3D) imaging techniques, Cone Beam Computed Tomography (CBCT) has become the preferred diagnostic modality for accurate orthodontic diagnosis and treatment planning. CBCT generates images with resolution ranging from 0.4 mm to 0.09 mm, which gives a precise reading and suffices the need for exactness of required measurements.[4], [5] Therefore, CBCT can prove to be instrumental in determining the linear and volumetric dimensions of the "Orthodontic Walls" from the root surface of the tooth. Thus, the relative change in thickness of alveolar bone complex can be evaluated following the desired orthodontic tooth movement.
The evidence demonstrating the consequence of retraction and intrusion of anterior teeth on the alveolar housing is very limited and controversial. Hence, more deliberation and evaluation of the topic is required. Therefore, the present study was designed with the aim to evaluate the change in the limit of maxillary dentoalveolar complex in terms of change in thickness mean area and volume, in cases planned for retraction and intrusion of maxillary anterior teeth. The study also evaluated the change in tooth length of maxillary anterior teeth to ascertain external apical root resorption (EARR), post-retraction and intrusion of maxillary anterior teeth.
Materials and Methods
The present study was a prospective observational study with a sample size of 15 subjects using a convenience sampling technique. Necessary ethical approval was obtained from the institutional review committee (IEC/OCT/2018 dated 22 Oct 2018) and written consent was obtained from the patients prior to commencement of the study. The following inclusion and exclusion criteria were considered for selection of subjects for the present study:
Inclusion criteria
Proclined maxillary incisors: Nasion - Point A to upper central incisor (1- NA) = 32°-40° & > 4 mm, ANB angle = 3°-7°, crowding of upper anterior = < 3 mm, overbite = 2-4mm, horizontal to average growth pattern and patients requiring retraction and intrusion of upper anterior.
Exclusion criteria
History of orthodontic treatment, history of periodontal surgery/ bone grafting in the maxillary anterior region, systemic diseases influencing bone metabolism and patients with known syndromic conditions including cleft lip and palate.
All subjects for the study were selected from the OPD of the Department after applying the inclusion and exclusion criteria. Standard orthodontic pre-treatment records (T0) were obtained for all subjects. The CBCT was obtained by using a machine manufactured by M/s Cefla Dental Group Italy, Model - NEW TOM GIANO: G-XR-46893. The CBCT data thus generated was stored in DICOM 3.0 format and transferred to HorosTM software (GNU Lesser general public license, Version 3 (LGPL-3.0), Horos Project, Annapolis, MD, USA) for assessment.
A standardised treatment protocol was followed for all the subjects and orthodontic records (T1) were obtained after three months of achieving the desired retraction and intrusion of maxillary anterior teeth.
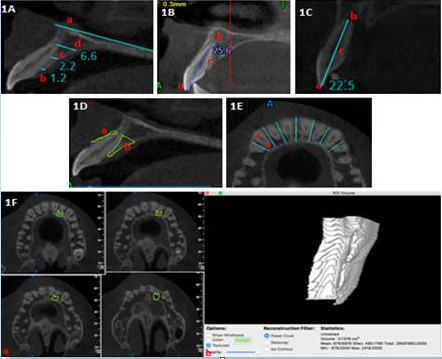
The thickness of maxillary dentoalveolar complex, tooth length and alveolar bone area measurements were done on a sagittal section of CBCT passing through the long axis of the tooth being assessed. The multiplane reformation (MPR) view of CBCT was used for the assessment of these parameters. The study parameters were assessed in relation to the maxillary central incisor, maxillary lateral incisor and maxillary canine of the right and left side, as these six teeth underwent a maximum change in position, during the course of treatment. The thickness of the maxillary dentoalveolar complex (buccal and palatal alveolar bone and cortices) was measured parallel to the palatal plane (ANS to PNS) at three levels - cervical, mid root and apical level of each of the six maxillary anterior teeth. The cervical level was marked equivalent to the crest of alveolar bone. The apical level was marked at apex of the root while the mid-root level was labelled at midpoint of the cervical and apical level. The overall thickness of alveolar bone was also measured at these three levels. [[Figure 1] A]. The length of maxillary anterior teeth was measured from incisal tip to apex of the root [[Figure 1] B]. If root resorption was evident, the tooth length was measured from the incisal edge to the midpoint of the line joining the buccal and palatal aspect of the resorbed/ blunted root apex [[Figure 1] C].
The buccal and palatal alveolar bone area was also calibrated using the HorosTM software by selecting the desired region of interest (ROI) [[Figure 1] D]. For assessing the buccal and palatal alveolar bone volume, the axial sections of CBCT were used. The maxillary anterior region (right side canine to left side canine) was divided into six segments by drawing lines perpendicular to buccal and palatal cortices passing through interdental region of each maxillary anterior tooth. Each of the six segments was further divided into two sub-segments (buccal and palatal) by drawing another line parallel to buccal and palatal cortices passing through centre of the maxillary anterior tooth being assessed [[Figure 1] E]. A series of ROIs were generated for each sub-segment from cervical region to root apex of the tooth in order to compute the alveolar bone volume around the tooth under assessment, using HorosTM software [[Figure 1] F].
The data at T(0) and T(1) was compiled in Microsoft Excel sheets [version Excel 2007(Windows), Microsoft Corporation One, Microsoft Way, Redmond, WA, USA]. The paired t-test was used to carry out an intra-group statistical comparison of means of continuous variables. The intra-class correlation (ICC) analysis was used to assess the intra and inter-observer variability for the continuous measurements between the measured data by two independent observers. Statistical Package for Social Sciences (SPSS version 21.0 Armonk, New York, USA: IBM Corp.) for Microsoft Windows was used to statistically analyze the complete data.
|
Parameter |
ICC - value for intra-operator agreement |
P-value |
ICC - value for inter-operator agreement |
P-value |
|
Alveolar bone thickness(mm) |
0.895 |
0.001*** |
0.824 |
0.001*** |
|
Alveolar bone area (mm2) |
0.902 |
0.001*** |
0.889 |
0.001*** |
|
Alveolar bone volume(cm3) |
0.885 |
0.001*** |
0.879 |
0.001*** |
|
Tooth length (mm) |
0.864 |
0.001*** |
0.845 |
0.001*** |
|
P-value by paired t test. P-value<0.05 was considered to be statistically significant. ***P-value<0.001. |
Results
The study sample consisted of fifteen subjects, a mixed Indian population of western Maharashtra, out of which eight were males and seven were females. The mean age of study sample was 18.1 ± 2.5 years. The mean proclination of maxillary incisors in the study sample was 34.1o ± 3.5o. Out of the fifteen subjects, six exhibited a horizontal growth pattern, while nine subjects had an average growth pattern. Five subjects showed ANB angle of 2o, seven subjects showed ANB angle of 3o while three showed ANB angle of 4o. In terms of crowding of teeth, eleven subjects exhibited no crowding, three subjects exhibited crowding of 2 mm while one subject had 1mm of crowding.
The data assessment for all subjects was carried out by the same operator. Eight randomly selected CBCT records were reassessed after one week by the same as well as by another trained operator in order to ascertain intra and inter-operator bias. The ICC analysis for all measurements: alveolar bone thickness, alveolar bone area, alveolar bone volume and tooth length had significantly higher ICC values (P-value<0.001 for all) which indicate statistically significant intra and inter-operator agreement for these parameters [[Table 1]].
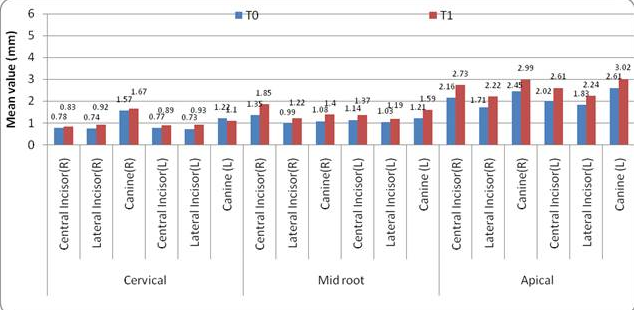
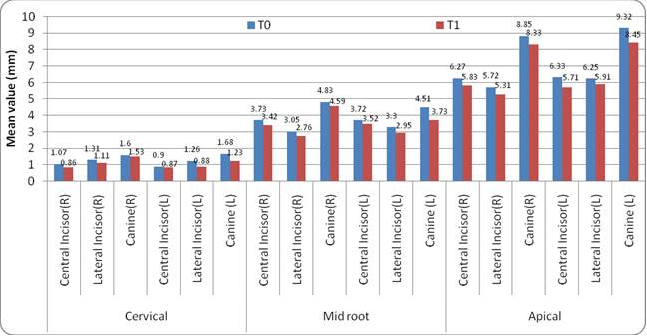
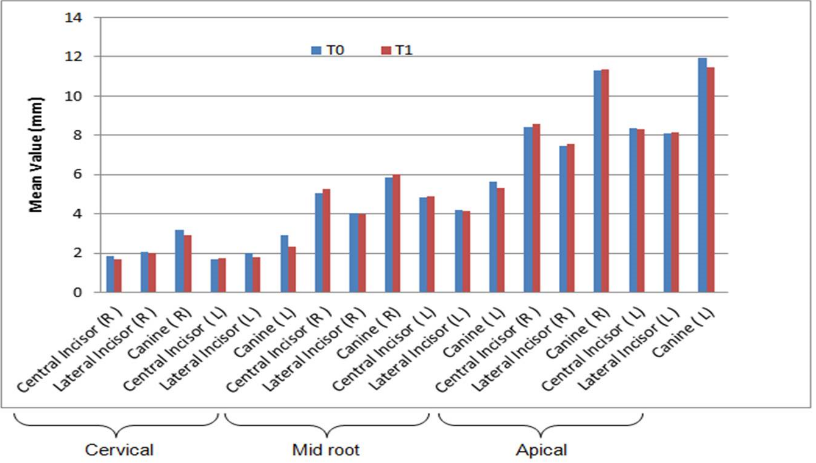
At T(1), the alveolar bone thickness of buccal side at cervical, mid root and apical level of all maxillary anterior teeth (except maxillary canine on left side) showed an increased thickness while the palatal side of all maxillary anterior teeth showed a reduction in alveolar bone thickness. The maxillary lateral incisor region showed a maximum increase (0.20 mm) in alveolar bone thickness at the cervical level while the maxillary central incisor region showed maximum increase in alveolar bone thickness along the mid-root and apical level (0.50mm and 0.59mm respectively) on the buccal side. The maxillary canine region showed maximum reduction in alveolar bone thickness at all three levels that is - cervical, mid root and apical level (0.45, 0.79 and 0.87 respectively) on the palatal side [[Figure 2], [Figure 3]]. The overall thickness of maxillary anterior alveolar bone, post retraction and Intrusion of maxillary anterior teeth was reduced. Maximum reduction in overall thickness was observed at the cervical region with minimal changes in thickness of alveolar bone at mid root and apical region. However, this change in overall thickness of maxillary anterior alveolar bone was not statistically significant (P >0.05) [[Figure 4]]
Change in alveolar bone mean area from T(0) to T(1)
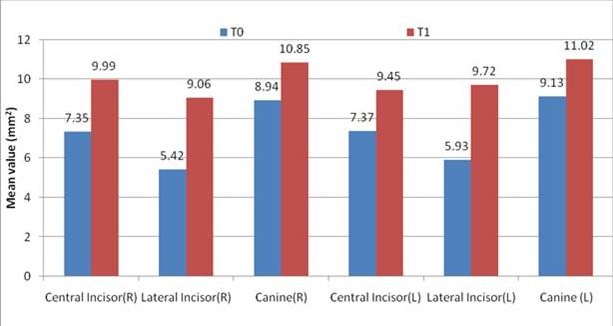
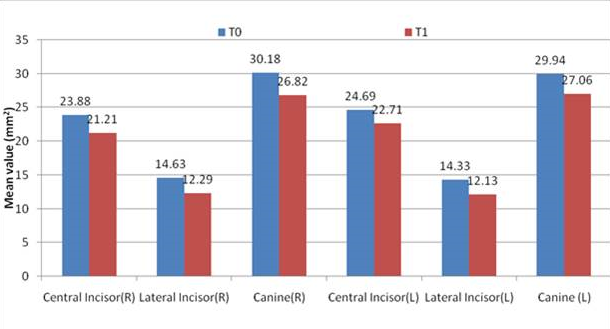
At T(1), the alveolar bone mean area on buccal side of all maxillary anterior teeth was increased significantly whereas palatal side showed significant reduction (P-value<0.05). A maximum increase in alveolar bone mean area on buccal side was observed in relation to lateral incisor (3.78 mm2) whereas the maximum decrease in alveolar bone mean area on palatal side was observed in relation to canine (3.36 mm2) [[Figure 5], [Figure 6]].
Change in alveolar bone volume from T(0) to T(1)
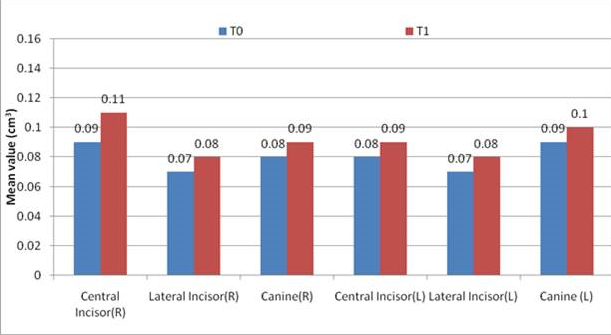
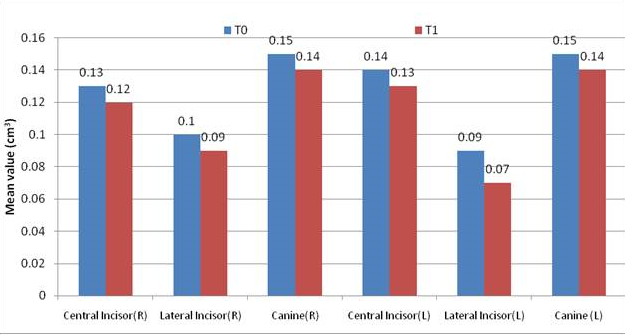
At T(1), the alveolar bone volume on the buccal side of all maxillary anterior teeth was increased significantly whereas palatal side showed significant reduction with respect to all six maxillary anterior teeth (P-value<0.05) [[Figure 6], [Figure 8]].
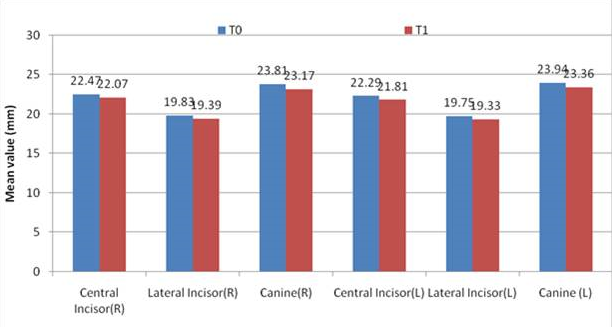
Change in tooth length from T(0) to T(1)
All six maxillary anterior teeth showed a reduction in total length of tooth as compared to pre-treatment measurements. However, the change in tooth length observed was statistically significant with respect to maxillary central and lateral incisors only [[Figure 9]].
Discussion
Orthodontic tooth movement is the result of the mechanical forces applied over the tooth that brings about the desired change in position of the tooth. Envelope of discrepancy[6] determines the limit of this desired change in tooth position, depending upon the type of treatment modality being used for obtaining the correction. The literature scan yields various studies that have studied the alveolar housing of a tooth that is the alveolar bone & its limits that influence the extent of orthodontic tooth movement (OTM). Moreover, the bone remodelling and tooth movement exhibited 1:2 ratio indicating that bone formation lags behind the bone resorption during OTM. This may lead to a reduction in the thickness of alveolar bone after OTM.[3], [7], [8] Even though the evidence of association of bone thickness reduction with tooth movement is present, the change in alveolar bone area or volume after orthodontic tooth movement lies unexplored. Since it is essential to consider the alveolar bone parameters in orthodontic diagnosis and planning of tooth movement; the concept of tooth movement-associated bone modelling and its quantification needs to be further investigated. Therefore, the present study was conceived in order to determine the change in linear and volumetric dimensions of buccal and palatal alveolar bone of maxillary anterior dentoalveolar segment while considering retraction and intrusion of maxillary anterior teeth and to observe the iatrogenic sequela (such as root resorption) associated with this change in alveolar bone.
Change in alveolar bone thickness
The thickness of alveolar bone present around the tooth, determines the limit of OTM.[6], [7], [8], [9] Variation in the thickness of this alveolar housing was observed with regard to the different types of malocclusion; therefore, affecting the extent of OTM in that particular type of malocclusion. [10], [11], [12], [13], [14], [15] Various studies have determined the change in alveolar bone thickness using lateral cephalogram, CT and CBCT using different linear and angular parameters.[1], [3], [9], [16], [17], [18], [19], [20], [21], [22], [23], [24] In the present study, the assessment of this change in the thickness of alveolar bone was done at three levels that are cervical, mid root and apical level on both buccal and palatal sides. Similar methodology and reference points were used by various other studies.[1], [3], [16], [17], [19] The present study observed a statistically significant reduction in the thickness of alveolar bone on palatal side at all three levels of all six maxillary anterior teeth. Maximum reduction was observed at cervical level on palatal side, especially maxillary central and lateral incisor. On the buccal side there was a significant increase in thickness observed at apical levels of six maxillary anterior teeth [[Figure 2], [Figure 3]]. Similar results were observed by various other studies that had used different 2D and 3D diagnostic modalities for assessing the change in alveolar bone thickness.[1], [3], [16], [17], [18], [19], [20], [21], [22], [23], [24] The similarity in the results between the present study and previously conducted studies may be attributed to similar demographic features of study sample, biomechanics, direction of OTM and reference points considered for assessment of changes. The literature scan could reveal only one study[20] that found no significant change in alveolar bone thickness post-retraction of anterior teeth. This deviation in result from present study may be an outcome of use of different treatment protocols, biomechanics and different reference points for measurement of alveolar bone thickness. Even though that study did not show significant change in alveolar bone thickness, a reduction in thickness of alveolar bone on palatal side alveolar bone and an increase on buccal side (maximum increase/decrease of 1.33 mm) was observed.[20] A systematic review by Sendyk M, et al.[8] on assessment of change in alveolar bone thickness showed evidence of significant reduction of alveolar bone thickness on palatal side following orthodontic tooth movement (mainly retraction of anterior teeth). The results of present study were found to be in accordance with that of this systematic review. The study sample, treatment setting and parameters used by present study were similar to the systematic review, which may be the probable reasons for identical result between these studies. The present study also shows reduction in overall thickness of maxillary anterior alveolar bone, following retraction and intrusion of maxillary anterior teeth, with maximum changes at cervical region. Similar results were observed by previous studies.[25], [26], [27] However, this reduction in overall thickness of maxillary anterior alveolar bone as observed in present study was statistically insignificant. Further, long term studies with larger sample size are recommended for better understanding on change in overall thickness of alveolar bone post retraction of anterior teeth.
Change in alveolar bone area
The alveolar bone area in the present study was calculated using CBCT assessment software HorosTM (Horos Project, Annapolis, MD, USA). The findings of present study exhibit significant decrease in alveolar bone area on palatal side and significant increase on buccal side of all six maxillary anterior teeth [[Figure 4], [Figure 5]]. Previous studies that determined the change in alveolar bone area following retraction of anterior teeth also found results that were matching with present study.[1], [25], [26], [27] The similarity in the findings may be a result of similar study sample characteristics along with the use of similar reference points for assessment of CBCT data. Various factors such as the effect of biomechanics, change in incisor inclination, displacement of apex, force level and direction of force application on alveolar bone has effect on the reduction in alveolar bone area.
Change in alveolar bone volume
The T0 and T1 alveolar bone volume in the present study was calculated using CBCT assessment software HorosTM (Horos Project, Annapolis, MD, USA). The present study revealed a significant reduction in alveolar bone volume on palatal side and a significant increase on buccal side with respect to all six maxillary anterior teeth as assessed using CBCT [[Figure 6], [Figure 7]]. There is no study available in contemporary literature that has measured and assessed changes in alveolar bone volume following retraction of anterior teeth. Thus, making the present study a pioneer attempt in this aspect.
Change in tooth length
EARR, bone dehiscence and fenestration are commonly observed side effects of orthodontic treatment.[28], [29] It is therefore essential to understand the pattern associated with these side effects so as to reduce their prevalence. The present study assessed the EARR as determined by change in tooth length, following retraction and intrusion of anterior teeth. The present study observed a significant reduction in tooth length with respect to maxillary central and lateral incisor following retraction and intrusion of maxillary anterior teeth. No significant reduction of tooth length was observed with maxillary canine [[Figure 8]]. Various other studies including systematic reviews that had assessed the EARR following OTM reveal increase incidence and severity of EARR when orthodontic forces were used for correction of malocclusion. A positive correlation between orthodontically induced root resorption and intrusive force was also established by the systematic reviews[1], [20], [29], [30], [31] Since in the present study, similar study sample characteristics and type of orthodontic tooth movement were considered, an equivalent outcome substantiating EARR was observed.
Clinical significance
The present study attempts to understand the changes in the dentoalveolar complex following retraction and intrusion of maxillary anterior teeth. The results of the present study show a significant reduction in alveolar bone thickness, area as well as volume on palatal side following retraction and intrusion of maxillary anterior teeth. Hence, tooth movement must be planned to ensure that the roots are well within the dimensions of available dentoalveolar bone, prior to planning for retraction of anterior teeth. This is crucial in order to avoid movement of tooth out of the alveolar housing, resulting in fenestration or dehiscence and possible increased mobility of teeth due to loss of supporting bone structure. The present study also exhibits a significant reduction in tooth length following retraction and intrusion of maxillary anterior teeth, suggestive of EARR. Therefore, it is essential to carefully plan or modify the biomechanics to be incorporated for desired tooth movement, so as to minimize these iatrogenic effects.
Limitations
The convenience sampling method was considered for sample calculation in the present study resulting in a relatively small sample size. It is recommended to confirm the results with a larger sample. The present study considered effect of a specific type of OTM (that is retraction and intrusion) on alveolar bone dimensions. The effect of other types of OTM on alveolar bone dimensions also requires detailed assessment. The alveolar bone dimensions are affected by various factors such as type of tooth movement, biomechanics, type of malocclusion, study sample characteristics, etc. However, assessment of effect of these individual factors was not considered in present study. The present study was conducted for a relatively short duration with results assessed at 3 months post-OTM. Long-term changes and stability of the results achieved cannot be established with this short duration of study. It is recommended to consider long-term follow-up of the results obtained. The exact force application on each tooth for retraction and intrusion of teeth was not calibrated in the present study. The amount and direction of force applied on a particular tooth are important factors responsible for achieving desired tooth movement. Any variation in force level or incorrect direction of force may result in side effects such as EARR, fenestration, dehiscence, etc.
Conclusions
The present study evaluated the change in the limit of maxillary dentoalveolar complex dimensions post-retraction and intrusion of maxillary anterior teeth. The following conclusions can be drawn from this study –
A significant reduction in thickness, mean area and volume of alveolar bone on palatal side (all three levels) and a significant increase on buccal side (apical level) was observed following retraction and intrusion of maxillary anterior teeth.
A significant decrease in tooth length of maxillary central and lateral incisors was observed, following retraction and intrusion of maxillary anterior teeth, suggestive of EARR.
It is therefore essential to assess the dimensions of alveolar housing prior to considering retraction and intrusion of anterior teeth in order to plan suitable biomechanics and treatment protocol which would minimize iatrogenic side effects and yield stable treatment outcomes. However, studies with larger sample size are recommended in order to obtain more realistic and reliable results, which would assist in orthodontic diagnosis and treatment planning.
Source of Funding
None.
Conflict of Interest
None.
References
- HW Ahn, SC Moon, SH Baek. Morphometric evaluation of changes in the alveolar bone and roots of the maxillary anterior teeth before and after en masse retraction using cone-beam computed tomography. Angle Orthod 2013. [Google Scholar]
- OP Kharbanda. . Orthodontics diagnosis and management of malocclusion and dentofacial deformities. 2nded 2013. [Google Scholar]
- A Singh, S Chandra, DK Agarwal, P Bhattacharya. A study to evaluate the alveolar bone thickness during anterior retraction using computed tomography. Int J Contemp Med Res 2017. [Google Scholar]
- P Mozzo, C Procacci, A Tacconi, PT Martini, IA Andreis. A new volumetric CT machine for dental imaging based on cone beam technique: preliminary results. Eur Radiol 1998. [Google Scholar]
- LA Feldkamp, LC Davis, JW Kress. Practical cone beam algorithm. J Opt Soc Am 1984. [Google Scholar]
- JL Ackerman, WR Proffit. Soft tissue limitations in orthodontics: treatment planning guidelines. Angle Orthod 1997. [Google Scholar]
- AD Vardimon, E Oren, Y Ben-Bassat. Cortical bone remodeling/tooth movement ratio during maxillary incisor retraction with tip versus torque movements. Am J Orthod Dentofac Orthop 1998. [Google Scholar]
- M Sendyk, DS Linhares, CM Pannuti, JB Paiva, R Neto. Effect of orthodontic treatment on alveolar bone thickness in adults: a systematic review. Dental Press J Orthod 2019. [Google Scholar]
- CS Handelmen. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod 1996. [Google Scholar]
- B Thilander. Dentoalveolar development in subjects with normal occlusion: a longitudinal study between the ages of 5 and 31 years. Eur J Orthod 2009. [Google Scholar]
- M Bajracharya. Analysis of maxillary bone thickness at incisor area in Class II div 1 malocclusion. Orthod J Nepal 2011. [Google Scholar]
- E Esenlik, FA Sabuncuoglu. Alveolar and symphysis regions of patients with skeletal Class II division 1 anomalies with different vertical growth patterns. Eur J Dent 2012. [Google Scholar]
- N Yodthong, C Charoemratrote, C Leethanakul. Factors related to alveolar bone thickness during upper incisor retraction. Angle Orthod 2013. [Google Scholar]
- MM Sadek, NE Sabet, I Hassan. Alveolar bone mapping in subjects with different vertical facial dimensions. Eur J Orthod 2015. [Google Scholar]
- YL Tian, F Liu, HJ Sun, P Lv, YM Cao, M Yu. Alveolar bone thickness around maxillary central incisors of different inclination assessed with cone-beam computed tomography. Korean J Orthod 2015. [Google Scholar]
- S Sarikaya, B Haydar, S Ciger, M Ariyurek. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofac Orthop 2002. [Google Scholar]
- K Nayak, A Shetty, MP Girija, R Nayak. Changes in alveolar bone thickness due to retraction of anterior teeth during orthodontic treatment: a cephalometric and computed tomography comparative study. Indian J Dent Res 2010. [Google Scholar]
- KY Nahm, JH Kang, SC Moon, YS Choi, YA Kook, SH Kim. Alveolar bone loss around incisors in Class I bidentoalveolar protrusion patients: a retrospective three-dimensional cone beam CT study. Dentomaxillofac Rad 2012. [Google Scholar]
- N Hacopian. Morphological changes in alveolar bone following orthodontic space closure. Loma Linda university electronic theses, dissertations & projects. 2015. [Google Scholar]
- TMF Oliveira, LV Claudino, CT Mattos. Maxillary dentoalveolar assessment following retraction of maxillary incisors: a preliminary study. Dental Press J Orthod 2016. [Google Scholar]
- SM Bae, HJ Kim, HM Kyung. Long-term changes of the anterior palatal alveolar bone after treatment with bialveolar protrusion, evaluated with computed tomography. Am J Orthod Dentofac Orthop 2018. [Google Scholar]
- PL Jarana, CM Diaz-Castro, A Falcao, C Falcao, JV Ríos-Santos, M Herrero-Climent. Thickness of the buccal bone wall and root angulation in the maxilla and mandible: an approach to cone beam computed tomography. BMC Oral Health 2018. [Google Scholar]
- SY Hong, JW Shin, C Hong, V Chan, UB Baik, YH Kim. Alveolar bone remodeling during maxillary incisor intrusion and retraction. Prog Orthod 2019. [Google Scholar]
- C Maspero, F Gauri, LO Castro, V Lanteri, A Ugolini, M Farronato. Correlation between dental vestibular-palatal inclination and alveolar bone remodeling after orthodontic treatment: a CBCT analysis. Materials 2019. [Google Scholar]
- EJ Son, SJ Kim, C Hong, V Chan, HY Sim, S Ji. A study on the morphologic change of palatal alveolar bone shape after intrusion and retraction of maxillary incisors. Sci Rep 2020. [Google Scholar] [Crossref]
- H Mao, A Yang, Y Pan, H Li, L Lei. Displacement in root apex and changes in incisor inclination affect alveolar bone remodeling in adult bimaxillary protrusion patients: a retrospective study. Head Face Med 2020. [Google Scholar] [Crossref]
- Q Sun, W Lu, Y Zhang, L Peng, S Chen, B Han. Morphological changes of the anterior alveolar bone due to retraction of anterior teeth: a retrospective study. Head Face Med 2021. [Google Scholar] [Crossref]
- ASK Chaitanya, YM Reddy, C Sreekanth, BV Reddy, BL Kumar, G Raj. Orthodontic tooth movements and its effects on periodontium. Int J Dent Med Res 2014. [Google Scholar]
- GA Mandelaris, R Neiva, L Chambrone. Cone-beam computed tomography and interdisciplinary dentofacial therapy: An American Academy of Periodontology best evidence review focusing on risk assessment of the dentoalveolar bone changes influenced by tooth movement. J Periodontol 2017. [Google Scholar]
- B Weltman, KWL Vig, HW Fields, S Shanker, EE Kaizar. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofac Orthop 2010. [Google Scholar]
- SD Currell, A Liaw, B Grant, PD Esterman, A Nimmo, . Orthodontic mechanotherapies and their influence on external root resorption: a systematic review. Am J Orthod Dentofac Orthop 2019. [Google Scholar]
- Introduction
- Materials and Methods
- Results
- Change in alveolar bone mean area from T(0) to T(1)
- Change in alveolar bone volume from T(0) to T(1)
- Change in tooth length from T(0) to T(1)
- Discussion
- Change in alveolar bone thickness
- Change in alveolar bone area
- Change in alveolar bone volume
- Change in tooth length
- Clinical significance
- Limitations
- Conclusions
- Source of Funding
- Conflict of Interest
