- Visibility 98 Views
- Downloads 11 Downloads
- DOI 10.18231/j.jco.2023.040
-
CrossMark
- Citation
Unilateral intrusion of extruded upper molar with use of transpalatal arch – A case report
Introduction
Overeruption of maxillary molars is a common finding caused by missing antagonist in adults or by failure of eruption in growing patient. Maxillary molar intrusion should be considered in such cases to re-establish the interarch space and enable adequate protraction of mandibular molars.[1], [2], [3] Several methods include elastics with removable appliances, E-chain or springs applied to palatal arches.[1] Skeletal anchorage for molar intrusion represented a major advancement; indeed, many authors have demonstrated excellent results from molar intrusion with miniscrew anchorage.[4], [5] We have used a modified transpalatal arch (TPA), that can easily intrude maxillary molars during orthodontic treatment.
Protraction of mandibular molars is challenging because of the high density of mandibular bone. There is often an inadequate dental anchorage in anterior region to protract even a single molar without reciprocal retraction of the incisors or deviation of dental midline. Miniscrews provide skeletal anchorage for mandibular molar protraction thereby avoiding the problems often encountered with dental anchorage. This article presents intrusion of extruded maxillary molar with use of modified TPA and mandibular molar protraction with miniscrews.[3]
Diagnosis and Treatment Plan
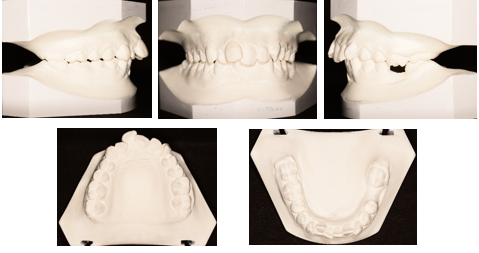
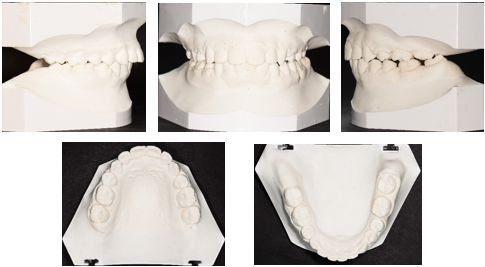
A 19-year-old female presented with anterior crowding and missing mandibular left first molar ([Figure 1]). Early loss of the molar had caused over eruption of the opposing first molar.
Clinical examination found a symmetrical mesofacial type. The patient had a convex profile, lip incompetence; the lower dental midline was deviated 2mm to the left. She had class I canine and molar relationship on the right side and end on canine relationship on the left side. Ellis class I fracture was observed in upper right central incisor. The mandibular plane was normal, no canting of the occlusal plane was observed. Model analysis indicated a symmetrical average maxillary and mandibular archform. Boltons tooth-size analysis found an anterior ratio of 78.1% (normal = 77.2% ± 1.6%), an overall ratio of 90.61% (normal 91.3% ± 1.9%). We noted 7mm of crowding in maxillary arch and 6mm of crowding in the mandibular arch ([Figure 1], [Figure 2] ).
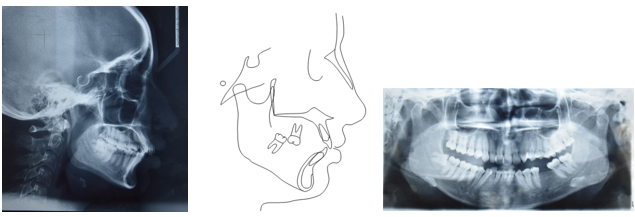
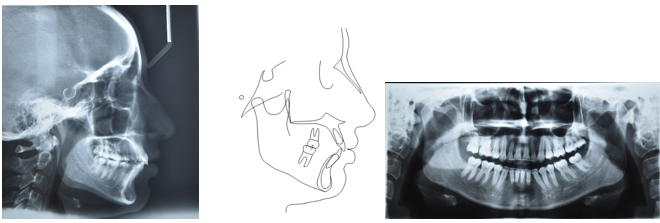
The panoramic radiograph revealed a normal trabecular bone pattern, good alveolar bone levels, and normal maxillary sinuses on both sides. The patient showed no signs or symptoms of TMD ([Figure 3]). Cephalometric analysis ([Table 1] ) confirmed a skeletal class II pattern (ANB = 5°, Wits appraisal = +3.5mm). The upper and lower incisors were proclined (UI-NA = 30°, 7mm; LI-NB = 29°, 6mm; LI-APog = 4mm), resulting in a reduced interincisal angle (124°).
Two treatment options were considered. First option included extraction of all first premolars to resolve the arch length deficiency followed by prosthesis in the mandibular left first molar region. The alternative option was to extract the upper first premolars to address the patient’s maxillary crowding and improve the soft tissue profile. Extraction of mandibular right first premolar and edentulous space of mandibular left first molar might have helped with the decrowding and retraction of lower anteriors followed by protraction of lower left second molar in the residual space. The patient accepted this option, as she denied replacement of missing molar with prosthesis.

|
|
Normal |
Pre-treatment |
Post-treatment |
Difference |
|
Skeletal |
|
|
|
|
|
SNA |
82° |
79° |
78° |
1° |
|
SNB |
80° |
74° |
74° |
0° |
|
ANB |
2° |
5° |
4° |
1° |
|
SN-MP |
32° |
33° |
33° |
0° |
|
FMA |
25°±4° |
26° |
26° |
0° |
|
Dental |
|
|
|
|
|
U1-NA(°) |
22° |
30° |
26° |
4° |
|
U1-NA(mm) |
4mm |
7mm |
4.5mm |
2.5mm |
|
U1-SN |
102°±2° |
109° |
105° |
4° |
|
L1-NB(mm) |
4mm |
6mm |
4mm |
2mm |
|
L1-NB(°) |
25° |
29° |
26° |
3° |
|
L1-MP |
90°±3° |
103° |
101° |
2° |
|
U1-L1 |
131° |
124° |
130° |
6° |
|
Soft tissue |
|
|
|
|
|
H-angle |
7°-15° |
22° |
21° |
1° |
|
Upper lip |
0-2mm |
2.5mm |
2mm |
0.5mm |
|
Lower lip |
0-2mm |
3mm |
2.5mm |
0.5mm |
Treatment Progress
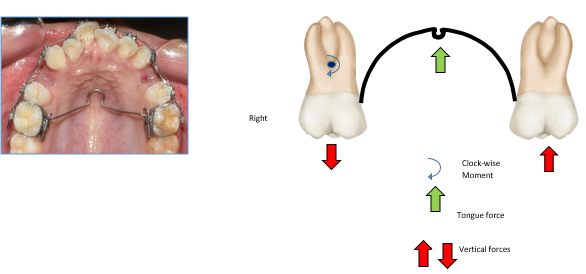
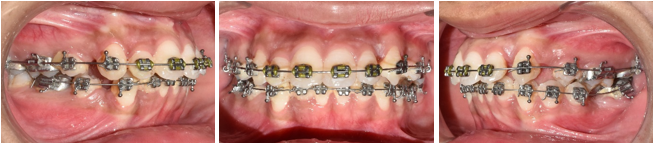
After banding the upper first molars, the remaining upper teeth were bonded (Roth-prescription .022″ × .028″ preadjusted edgewise appliance) and a low-placed transpalatal arch with buccal crown torque was placed on upper right first molar ([Figure 4]). During six months of levelling upper second molars were banded and .014″, .016″, .016″ × .022″ nickel titanium archwires were used in the upper arch ([Figure 5]). Following the intrusion of upper left first molar and alignment of upper arch, the lower arch was bonded. Levelling was initiated using .016″, .016″ × .022″ nickel titanium archwire and complete alignment using .016″ × .022″ stainless steel archwires. After eleven months of alignment, retraction of maxillary canine was performed on .019″ × .025″ stainless steel wire using NiTi closed coil spring (9 mm; Ormco, Orange, Calif)6 ([Figure 6]). Meanwhile a self-drilling 1.2mm × 8mm miniscrew (3M Unitek) were then inserted into the mandibular buccal alveolar bone distal to the first premolars on left side, without mucoperiosteal incisions or flaps ([Figure 7]) in order to reinforce the dental anchorage unit. Buccal hook for auxiliary tube was fabricated chairside using .019″ × .025″ stainless steel and protraction force on lower left second molar was given by elastomeric chain on .019″ × .025″ stainless steel arch wire (American Orthodontics) to provide force.
Due to trans-septal fiber pull and mesioocclusal direction of eruption, the lower left third molar drifted into the space of the lower left second molar without any separate mechanics.
Eighteen months later, residual spaces were closed using double key hole loop made of .019″ x .025″ stainless steel wire in upper arch ([Figure 8]) and elastomeric chains in lower arches, following which a panoramic radiograph was taken to evaluate root parallelism.[6] Brackets were then repositioned, and .016" × .022" copper nickel titanium archwires were placed.
After three months of finishing and detailing another two months of settling was done on upper and lower .014″ NiTi, but the patient's insistence on removing the appliance earlier for personal reasons resulted in left out space distal to Mesialized lower left second molar and root divergence of lower right and left canine. Following which case was debonded and enameloplasty was done in upper right central incisor. A 2-2 fixed bonded retainer in the upper and 3-3 fixed bonded retainer in the lower arch was given to the patient.



Treatment Results
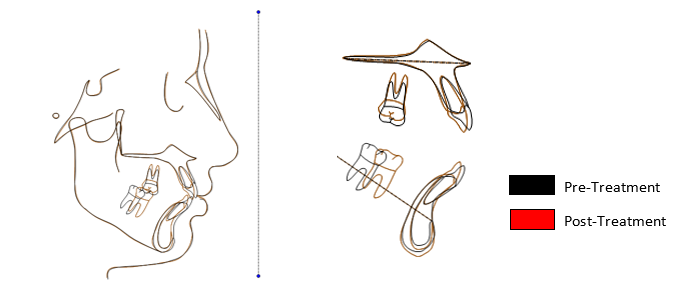
After twenty-three months of treatment, all objectives were achieved ([Figure 9]). A significant improvement in the facial profile was produced by retraction of the upper lip, which in turn corrected the lip incompetence ([Table 1]). This effect was attributable to retraction of the upper incisors and their subsequent realignment in the maxillary bone. A consonant smile arc was observed. Class I molar and Class I canine relationship was maintained on right side and Class II molar relationship, with Class I canine relationship on the left side was obtained. The incisors were positioned with normal overjet, overbite and good posterior interdigitation ([Figure 9], [Figure 10]). The maxillary cephalometric superimposition indicated that the upper left molar was intruded, and the upper incisors were retracted. The mandibular superimposition showed that the lower left molar was mesialized, and the lower incisors were retracted ([Figure 12]). The orthopantomogram revealed root divergence in lower right and left canine which may cause an open gingival embrasure. Repositioning the bracket can be performed to converge the roots to eliminate black triangles.[7] However, there is one-year follow-up record ([Figure 13]) of the case showing that, teeth positions were stable. Residual space of 2mm distal to mesialized lower left second molar may lead to food lodgment and compromise the periodontal health. For which the importance of plaque control and good oral hygiene must be stressed to the patient.


Discussion
Compared to conventional banded TPAs which serves for anchorage, a minor modification, requiring only a few minutes of chair side time can serve as noninvasive and inexpensive procedure which offers several advantages for intrusion of a supraerupted upper first molar along with anchorage.[8] Although miniscrews have been shown to provide safe and efficient anchorage for intrusion of overerupted molars, using forces from elastic chains or coil springs, without affecting adjacent teeth.[9], [10] TPAs does not rely on patient compliance, for success unlike TADs due to oral hygiene and bone quality. Also, it causes less discomfort compared to a palatal miniplate.[11]
With the concept of third order activation of only one insert will produce a unilateral couple and result in a buccal crown torque on that molar and an associated equilibrium force on the other molar. The associated equilibrium forces will be in a vertical (intrusive-extrusive) direction. The molar with the large buccal crown torque moment will also feel an extrusively directed equilibrium force applied at the sheath. The contralateral molar will have an intrusive equilibrium force acting at the sheath.[12] Therefore, extrusive force on upper right first molar might have counterbalanced by intrusive force of tongue on low placed TPA ([Figure 4]).
In the case shown here, the maxillary first premolars were extracted to allow two-phase upper anterior retraction to gain space for anterior decrowding. Maspero and colleagues found no difference between one and two-phase retraction in terms of treatment outcome, except that there was less incisor trauma.[13]
Patients with missing teeth have two treatment options, substitution by natural teeth or replacement by prosthesis. Natural teeth substitution can be an effective, aesthetic treatment choice for missing teeth replacement. [14] Kyung et al [15] reported a 9-mm mesial movement of mandibular second molars, and Nagaraj et al [16] reported an 8-mm movement using miniscrews to close bilateral missing mandibular first molar spaces. Protraction of second molar orthodontically in space of missing first molar gives superior alveolar bone support and oral hygiene than conventional prosthesis. Raveli et al [17] showed that that orthodontic tooth movement is an effective method for reclaiming new alveolar bone. Molar protraction requires anchorage. In cases where anchorage is insufficient, root resorption and molar tipping occur. [18] Avoiding anchorage loss in the mandible is significantly more difficult than maxilla, owing to anatomic jaw variations. The rate of molar protraction is inversely related to the radiographic density or cortical thickness of the resisting bone, because of the increased thickness of mandibular cortical bone, the rate of mandibular molar translation with skeletal anchorage is nearly half that of maxillary molar. [19] Bone density (or bone quality), peri-implant soft tissue health, adequacy of peri-implant bone stock, and operator technique are the main biological determinants of miniscrew stability. [20] Despite the higher failure rate of mandibular miniscrews, probably due to root proximity have been recorded. In this case, there was no breakage or miniscrew failure.
The patient reported no pain after miniscrew placement, substantiating a report by Kuroda and colleagues in which miniscrews inserted without flap surgery were associated with less pain and discomfort. [21] Inserting the miniscrew between the lower left first and second premolar along with buccal hook from molar tube allowed the force to pass close to the center of resistance, therefore the molars could be protracted without tipping. Immediately after placement of miniscrew, the protraction force was applied from the second molar buccal hook to TAD.
Lower lip to E-line, ANB angle, and extraction pattern were the pretreatment variables that were most predictive of a good facial profile. In this case, we chose to extract upper first premolars because of the excessive crowding. For two-phase anterior teeth retraction, where maximum anchorage was planned, upper second molars were banded to enhance the posterior anchorage unit. Lower right first premolar was extracted along with space due to missing lower left first molar, to resolve crowding in the mandibular arch. Good root paralleling and minimal root resorption was achieved, as seen on the post-treatment panoramic radiograph and lateral cephalogram.
Conclusion
A modified TPA is a simple method of intruding overerupted maxillary molars with the advantage of patient comfort, reduce chairtime and cost-effectiveness.
Protraction of second molars into first molar space with TADs is a conservative and cost efficient alternative as compared to prosthetic rehabilitation. The patient is saved from added implant surgeries, related complications.
Source of Funding
None.
Conflict of Interest
None.
References
- A Enacar, M Pehlivanoglu, CA Akcan. Molar intrusion with a palatal arch. J Clin Orthod 2003. [Google Scholar]
- F Torsello, M Turchi, M Cordaro. Molar intrusion using clear aligners without additional anchorage devices. J Clin Orthod 2021. [Google Scholar]
- ND Kravitz, T Jolley. Mandibular molar protraction with temporary anchorage devices. J Clin Orthod 2008. [Google Scholar]
- YC Park, SY Lee, DH Kim, SH Jee. Intrusion of posterior teeth using mini-screw implants. Am J Orthod 2003. [Google Scholar]
- ND Kravitz, B Kusnoto, TP Tsay, WF Hohlt. The use of temporary anchorage devices for molar intrusion. J Am Dent Assoc 2007. [Google Scholar]
- M Kumar, M Goyal, A Kushwah. A Review on Double Keyhole Loop. TMU J Dent 2018. [Google Scholar]
- NA Meeran. Iatrogenic possibilities of orthodontic treatment and modalities of prevention. J Orthod Sci 2013. [Google Scholar]
- JM Hudson. Tongue-friendly transpalatal arches. J Clin Orthod 2000. [Google Scholar]
- AG Crismani, MH Bertl, AG Celar, HP Bantleon, CJ Burstone. Miniscrews in orthodontic treatment: Review and analysis of published clinical trials. Am J Orthod 2010. [Google Scholar]
- A Purkayastha, R Mohanty, S Panda, U Das. Miniscrew implants for intrusion of supraerupted molar: A noninvasive approach for space regaining. Contemp Clin Dent 2019. [Google Scholar]
- V Pattabiraman, R Sood, S Sabrish, O Rizvi. Intrusion of Supraerupted Second Molars with the Palatal Intrusion Fork. J Clin Orthod 2015. [Google Scholar]
- J Rebellato. Two-couple orthodontic appliance systems: transpalatal arches. Semin Orthod 1995. [Google Scholar]
- C Maspero, G Galbiati, L Giannini, G Guenza, M Farronato. Class II division 1 malocclusions: Comparisons between one- and two-step treatment. Eur J Paediat Dent 2018. [Google Scholar]
- VO Kokich, GA Kinzer. Managing congenitally missing lateral incisors. Part I: Canine substitution. J Esthet Restor Dent 2005. [Google Scholar]
- SH Kyung, JH Choi, YC Park. Miniscrew anchorage to protract lower second molars into first molar extraction sites. J Clin Orthod 2003. [Google Scholar]
- K Nagaraj, M Upadhyay, S Yadav. Titanum screw anchorage for protraction of mandibular second molars into first molar extraction sites. Am J Orthod Dentofac Orthop 2008. [Google Scholar]
- TB Raveli, DB Raveli, KC De Mathias Almeida, A Pinto. Molar uprighting: A Considerable and safe decision to avoid prosthetic treatment. Open Dent J 2017. [Google Scholar]
- ML Stepovich. A clinical study on closing edentulous spaces in the mandible. Angle Orthod 1979. [Google Scholar]
- WE Roberts, GR Arbuckle, M Analoui. Rate of mesial translation of mandibular molars using implant-anchored mechanics. Angle Orthod 1996. [Google Scholar]
- HS Park, SH Jeong, OW Kwon. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofac Orthop 2006. [Google Scholar]
- S Kuroda, Y Sugawara, T Deguchi, HM Kyung, TT Yamamoto. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am J Orthod 2007. [Google Scholar]
