- Visibility 466 Views
- Downloads 41 Downloads
- Permissions
- DOI 10.18231/j.jco.2025.003
-
CrossMark
- Citation
Comparative analysis of orthodontic adhesives for bracket bonding reliability: A systematic review
Abstract
Background: The effectiveness of adhesive materials used for bracket bonding is an important factor of orthodontic treatment that directly affects patient satisfaction and treatment success. It is important to know the advantages of various orthodontic adhesives to improve treatment results and reduce issues like enamel demineralization.
Aim: To thoroughly evaluate and contrast the performance of different orthodontic adhesives in terms of enamel protection and bonding stability throughout orthodontic therapy.
Materials and Methods: Following PRISMA criteria, a systematic search was carried out using several databases, including PubMed, Scopus, Web of Science, and the Cochrane Library. Medical Subject Headings (MeSH) terms and carefully chosen keywords were used in the search technique to find pertinent research published between 1989 and 2023 that included approximately 1465 total articles. The inclusion criteria covered studies that evaluated the efficacy of orthodontic adhesives for the reliability of bracket bonding and the preservation of enamel during orthodontic treatment.
Results: Six recognized papers that evaluated the efficacy of diverse orthodontic adhesives using disparate approaches. The results showed that different adhesive types varied in bonding strength, failure rates, cleanup times, and enamel protection. Significant distinctions were noted between adhesives that were chemically cured and those that were light-cured, as well as between adhesives based on resin and glass ionomer cement. While retaining a good bonding strength, compomer and composite resin adhesives shown potential benefits in lowering enamel decalcification.
Conclusion: The significance of taking clinical results and bonding performance into account when choosing adhesive materials for orthodontic treatment is highlighted by a comparative examination of orthodontic adhesives. To improve treatment efficacy and patient care, future research efforts should concentrate on overcoming methodological constraints and further clarifying the mechanisms behind enamel protection and adhesive bonding strength.
Introduction
Orthodontic treatment entails a multifaceted interplay of methodologies and materials with the overarching goal of attaining ideal dental alignment and occlusion. The secure bonding of orthodontic brackets onto the tooth surface plays a pivotal role that significantly influences treatment efficiency and patient satisfaction. Also, maintaining the integrity of enamel amidst the complexities posed by fixed orthodontic appliances stands as a primary apprehension for dental practitioners. Thus, the meticulous selection and assessment of orthodontic adhesives and sealants assume a critical role in ensuring the efficacy and safety of orthodontic procedures.
Evaluation of orthodontic adhesives
The goal of achieving better patient outcomes and performance has led to a noticeable change in orthodontic adhesive solutions throughout time.[1] Prior until recently, primer-based adhesives were the go to choose for bracket bonding because of their consistent adherence, which is achieved by a multi-step application procedure. But the intrinsic complexity associated with primer-based systems has spurred research into substitute formulations meant to make the bonding procedure simpler. As viable substitutes, more recent non-primer adhesives are starting to emerge; they provide robust bond strength and simplified application procedures.[1], [2], [3] explores how historical development and technical breakthroughs have shaped modern bonding procedures in orthodontics in his groundbreaking study. The authors sheds insight on the reasons and ramifications behind significant changes in adhesive formulas and application techniques through painstaking investigation. They give insightful explanations of the historical background and the motivations behind the creation of innovative non-primer adhesives, which have the potential to completely transform bracket bonding procedures. This academic investigation deepens the general understanding of the complex interactions that exist between technology advancement, historical precedence, and orthodontic bonding clinical practice.
Challenges in enamel protection
During orthodontic treatment, preventing or reducing enamel decalcification, also called white spot lesions, is a continuous challenge that requires ongoing efforts. Different resin sealants have been used to protect enamel integrity, with few of them exhibiting potential in reducing enamel destruction. Yet, the reduction of sealant material from brushing teeth and wear from chewing presents a major concern in clinical settings and creates a hurdle for product developers.[2], [4], [5], [6], [7] Orthodontic therapy is essential for improving tooth alignment and appearance, but it also poses serious risks to the integrity of the enamel. The presence of fixed appliances increases the likelihood of enamel demineralization and the formation of white spot lesions by fostering an environment that is favorable to plaque accumulation.[8], [9], [10], [11], [12], [13], [14], [15] A multimodal strategy that incorporates proactive enamel protection techniques and efficient bonding materials is required to mitigate these issues. In this situation, sealants and bonding materials play critical functions, serving as barriers that prevent acid erosion and promoting the remineralization processes that maintain dental integrity.[8], [15], [16], [17], [18], [19], [20], [21]
Clinical considerations, current landscape
When choosing orthodontic adhesives and sealants, clinicians must balance several parameters, including bond strength, application ease, and long-term efficacy. Studies have attempted to clarify how various adhesive formulations behave in comparison to one another and how this affects clinical results. Important information about enamel demineralization hazards, bracket bond failure rates, and the mechanical characteristics of different adhesive systems may be found in pilot studies, systematic reviews, and meta-analyses. The state of adhesive technology and enamel preservation techniques is changing along with the orthodontics sector. Continuous research endeavours are directed at improving current formulas, streamlining bonding procedures, and creating novel materials that cater to the changing requirements of orthodontic applications. Moreover, multidisciplinary partnerships involving materials scientists, dental researchers, and orthodontists have the potential to further our knowledge of the physiology of enamel and adhesive biomechanics, which will improve treatment outcomes and patient care.
As a result, orthodontic sealants and adhesives are essential parts of modern orthodontic treatment, helping to maintain the integrity of enamel and enable the safe attachment of brackets. The significance of evidence-based methods in clinical decision-making is highlighted by the advancement of adhesive technology and a better comprehension of the mechanisms underlying enamel demineralization. In addition to offering a thorough overview of the state of orthodontic adhesives and sealants today, this systematic review also attempts to identify areas for further research and innovation by combining clinical perspectives and research findings.
The primary goals of this systematic review were to compare and thoroughly assess the effectiveness of sealants in preventing enamel demineralization during fixed orthodontic treatment, as well as the efficacy of different orthodontic adhesives for bracket bonding reliability. By means of a comprehensive synthesis of extant literature, the review aimed to clarify the subtle distinctions between primer-based and non-primer adhesives, as well as their corresponding effects on the failure rates of bracket bonds. Thus, the present review was attempted to examine how sealants and bonding materials can reduce the likelihood of enamel demineralization, giving clinicians important information while choosing the best materials for orthodontic treatments. The primary aim of this systematic review was to ascertain the improvement in the patient outcomes and evidence-based practice in orthodontics by compiling various study findings and analysing their research work.
Materials and Methods
Research question
How effective are sealants and orthodontic adhesives in protecting enamel during orthodontic treatment, and how effective are they in gluing brackets together?
Timeline of the study: 1989 to 2023.
Search strategy
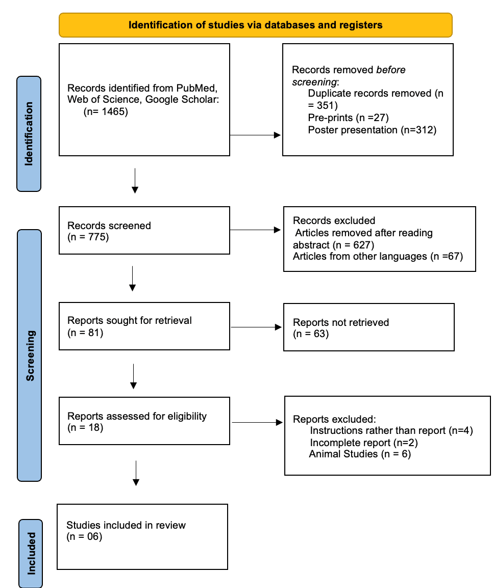
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria were followed during the search procedure to guarantee repeatability and transparency ([Figure 1]). A comprehensive search of the literature was carried out using several internet databases, including the Cochrane Library, PubMed, Scopus, and Web of Science. Medical Subject Headings (MeSH) terms and well-chosen keywords were combined in the search strategy to maximize the retrieval of pertinent studies. Several databases, including PubMed, Scopus, Web of Science, and the Cochrane Library, were searched. The important keywords that were used for the search a broad range of literature on orthodontic adhesives, sealants, and enamel protection during orthodontic treatment included: "bracket bonding", sealants", enamel protection", and "orthodontic treatment", and “enamel demineralization", “decalcification”, success rates”, “failures orthodontic brackets”, and “orthodontic adhesives”, “composite resin adhesives”, “glass ionomer cement”, “sealants”. These keywords were also used in variations to cover a wide range of pertinent studies. The search approach combined MeSH terms and keywords to find all relevant literature on the subject. This thorough technique made sure that no pertinent research was missed during the search. Following the recommendations of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), the study preserved search strategy rigor and transparency. All things considered, the systematic search over several databases made it easier to find a wide variety of research for further screening and incorporation into the systematic review.
|
Author/year |
Study methodology |
No. of brackets placed |
Adhesive type |
% of brackets failure |
Adhesive Bonding Outcome: Variations & Effects |
|
O’brien et al., n.d. |
In this clinical trial, 52 patients aged 13 to 29 years underwent fixed appliance treatment, with a total of 542 bracket bases placed. Two bracket base designs were employed: a foil mesh and an indented, photo-etched base. Patients received either a light-cured material or a chemically cured adhesive. Each patient was randomly assigned two different bracket/adhesive combinations for each side of the mouth. Bracket bonding techniques were standardized, involving specific steps for each adhesive type. |
542 |
Light-Cured Material Chemically Cured |
4.7% 6.0% |
The overall failure rate of adhesives that are chemically and light-cured is comparable. There were no discernible variations between the adhesives and bracket base kinds.For every adhesive/base combination, the rate of posterior tooth failure was greater (p < 0.001). More time for positioning and improved handling qualities are provided by light-cured materials. |
|
Norevall et al., 1996 |
60 orthodontic patients, ages 10 years 8 months to 19 years 1 month, participated in the clinical experiment. For bracket bonding, they were randomized to receive either no-mix diacrylate or glass ionomer cement (GIC), and the brackets were further divided into mesh foil bases and machine-cut grooves. Each type of glue had its own set of procedures for bonding and debonding. When compared to diacrylate, GIC demonstrated lower clean-up times but greater bracket failure rates, underscoring both the benefits and drawbacks of this material for orthodontic bonding. |
60 (30 brackets per group) |
GIC and Diacrylate |
GIC: 36%, Diacrylate: 15% |
The clinical trial's adhesive agent bonding results showed that glass ionomer cement (GIC) and diacrylate differed significantly from one another. Compared to diacrylate, which had a bracket failure rate of 15%, GIC showed a higher rate of 36%. These results also highlighted notable differences in failure rates throughout bracket kinds. Even though GIC adhered to enamel surfaces a little better, it also showed a far faster cleanup time following debonding. All things considered, even while GIC raised the possibility of bracket failures during treatment—especially when combined with a cut groove base type—it also had the benefit of requiring less time to clean enamel surfaces. |
|
Summers et al., 2004 |
The purpose of this study was to examine the in vivo survival rates of orthodontic brackets joined with a standard resin adhesive (Light Bond) bonded with 37% phosphoric acid and brackets glued with resin-modified glass ionomer adhesive (Fuji Ortho LC) after conditioning with 10% polyacrylic acid. It also aimed to compare the two adhesives' in vitro bond strength, identify the mode of bracket failure based on adhesive remnant index (ARI) testing conducted both in vivo and in vitro, and compare the changes in enamel surface morphology following etching or conditioning using scanning electron microscopy (SEM). |
Brackets were bonded to 50 extracted premolars, while in the in vivo study, 398 teeth were bonded in 22 subjects using a split-mouth technique. |
Two adhesive types were used: |
There were notable variations in the in vitro study's shear bond strengths and debond periods between the adhesives. Comparing Light Bond against Fuji Ortho LC, the former showed noticeably stronger bonds. After 1.3 years, there were no appreciable variations in bracket failure rates between the two adhesives in the in vivo trial. |
According to the in vitro investigation, Light Bond outperformed Fuji Ortho LC in terms of shear bond strengths. Nonetheless, after 1.3 years, the in vivo investigation revealed comparable survival rates for the two adhesives, indicating that resin-reinforced glass ionomers can offer sufficient binding strengths in clinical settings. It may be simpler to clean up after debonding since Fuji Ortho LC and enamel have a weaker chemical bond. According to SEM examination, conditioning with 10% polyacrylic acid resulted in a smoother enamel surface than etching with 37% phosphoric acid. |
|
Millett et al., 2000 |
The purpose of this clinical experiment was to compare the cariostatic capability and survival duration of resin adhesive and compomer when used to adhere stainless steel orthodontic brackets to teeth in the labial region. A random selection process was used to choose 45 consecutive patients receiving fixed appliance therapy. 426 brackets (213 composite, 213 resin adhesive) were bonded alternately on either side of the mouth in a split-mouth configuration. Patient details were noted, such as age, sex, and kind of malocclusion. Standardized protocols were followed for the bonding of brackets, and color transparencies taken before and after treatment were used to measure decalcification using a caries index. |
426 brackets were placed, with 213 bonded using compomer and 213 with resin adhesive, in a split-mouth design. |
Two adhesive types were used: - Right-On, a no-mix resin adhesive, served as the control, while - Dyract Ortho, a light-cured compomer resin, was the test agent. |
17% for compomer and 20% for resin adhesive, showing comparable performance between the two. |
The survival time distributions of brackets bonded with resin adhesive and brackets bonded with compomer adhesive did not differ significantly. Patient age at treatment onset proved to be a good predictive factor, while patient sex and malocclusion type had no significant impact on bracket survival. Comparing compomer-bonded brackets to resin adhesive-bonded brackets, the former showed noticeably reduced decalcification, suggesting a possible benefit in cariostatic qualities. |
|
Rao et al., 2013 |
Using an in vitro methodology, the study assessed orthodontic bonding agents away from living organisms. To be tested over the course of one hour and twenty-four hours, 150 premolar teeth were randomly split into five major groups, each of which was further divided into two subgroups. The study looked at three different types of adhesives: conventional glass ionomer cement, resin-reinforced glass ionomer cement, and composite resin. Shear bond strength was measured using a universal testing device, and bonding techniques varied throughout subgroups. |
150 premolar teeth |
Composite resin, Resin Reinforced Glass Ionomer Cement, Conventional Glass Ionomer Cement |
Not applicable |
After one and two days, composite resin showed a greater shear bond strength than both varieties of glass ionomer cement. For every group, the shear bond strength rose throughout a 24-hour period. In comparison to regular glass ionomer cement, resin-reinforced glass ionomer cement demonstrated a greater binding strength. Polyacrylic acid conditioning greatly increased the resin-reinforced glass ionomer cement's binding strength. |
|
Ramsundar et al., 2023 |
The bracket failure rates of a novel primerless orthodontic glue were compared to those of a traditional primer-based orthodontic adhesive in this split-mouth randomized pilot study. Angle's class I or II malocclusion affected fifteen orthodontic patients. All patients received metal bracket-equipped fixed orthodontic appliances. Orthofix SPA (primerless adhesive) and Transbond XT (primer-based adhesive) were used alternatively for bonding in the quadrants. Standardized protocols were followed for the enamel etching, bonding, and oral prophylaxis. Patients were instructed to return any debonded brackets to the hospital after checking them every day. For three months, there was a reassessment every four weeks. |
300 brackets were placed, with 152 bonded using Orthofix SPA (primerless adhesive) and 148 with Transbond XT (primer-based adhesive). |
Two adhesive types were used: • Orthofix SPA (primerless adhesive) and • Transbond XT (primer-based adhesive). |
Overall bracket failure rate was 8.6%, with 6.3% in the Orthofix SPA group and 2.3% in the Transbond XT group. No statistically significant inter-group difference was observed. |
There was no discernible difference between primerless and primer-based glue in terms of the number of bracket failures that occurred. Premolars and mandibular canines showed greater bracket failure rates, though not to a statistically significant degree. |
|
Author/year |
Adhesive type used |
% of brackets used |
Adhesive Performance Analysis |
|
O’brien et al., n.d. |
Light-Cured Material |
4.7% |
Comparable failure rates between chemically and light-cured adhesives. |
|
Norevall et al., 1996 |
Glass Ionomer Cement (GIC) |
36% |
Higher failure rate compared to diacrylate, faster cleanup time. |
|
Summers et al., 2004 |
Light Bond (Conventional Resin) |
6.0% |
Significantly greater shear bond strengths compared to Fuji Ortho LC in vitro. |
|
Millett et al., 2000 |
Compomer |
17% |
Comparable performance to resin adhesive with potentially reduced decalcification. |
|
Rao et al., 2013 |
Composite Resin |
Not applicable |
Greater shear bond strength than both varieties of glass ionomer cement. |
|
Ramsundar et al., 2023 |
Orthofix SPA (Primerless) |
6.3% |
No significant difference compared to primer-based adhesive in bracket failure rates. |
Inclusion criteria
Research assessing orthodontic adhesives' effectiveness for dependable bracket bonding.
Studies examining how well sealants preserve enamel while undergoing orthodontic treatment.
Published in peer-reviewed journals, randomised controlled trials (RCTs), observational studies, systematic reviews, and meta-analyses.
Research is available in English.
Articles that were released between 1989 to 2023 to guarantee that current research is included and to give an adequate amount of time for examination.
Exclusion criteria
Research unrelated to the effectiveness of orthodontic glue or enamel preservation during orthodontic therapy.
Articles in languages other than English.
Editorials, conference abstracts, case reports, and animal research.
Data extraction, synthesis, and quality assessment
Three reviewers, AKS, DR and VR, extracted data independently using a standardized form that included study characteristics, design, sample size, intervention details, outcomes, and major results. While DR focussed on the specifics of the intervention and the outcome measures, AKS focused on extracting data pertaining to the study design and sample characteristics. Key findings extraction and maintaining uniformity in data extraction across research were under VR's purview. The reviewers discussed and came to a consensus on any differences or opinions. Using the appropriate instruments based on research design, such as the Cochrane risk of bias tool for randomized controlled trials (RCTs), the quality of the included studies was assessed. For every study, AKS and DR carried out an independent quality evaluation, evaluating a range of areas including reporting bias, attrition bias, performance bias, detection bias, and selection bias. VR verified the accuracy and dependability of the quality assessment results by cross-validating them. Reviewers convened to discuss and reach a consensus on differences in quality evaluation. Compiling the gathered data and presenting the most important discoveries was the process of data synthesis. Close collaboration between AKS, DR and VR allowed for the synthesis of both quantitative and qualitative data. While qualitative data were narratively synthesized, quantitative data were evaluated using the proper statistical techniques. All three reviewers performed subgroup analyses to examine study heterogeneity and pinpoint possible sources of variation. The reviewers sought to give a thorough examination of the relative efficacy of orthodontic adhesives and sealants for enamel protection and bracket bonding reliability during orthodontic treatment through cooperative efforts and careful data synthesis.
Risk of bias assessment
Risk of bias assessment assessed potential biases and the quality of the methodology. This involved evaluating areas including reporting bias, attrition bias, detection bias, performance bias, and selection bias. Two reviewers carried out the assessment separately, and disagreements were settled by discussion or, if needed, by involving a third reviewer.
To summarize, a structured methodology was used in this systematic review, which included a thorough literature search, strict selection criteria, transparent data synthesis, standardized data extraction and quality assessment, and a thorough risk of bias assessment. The study sought to offer a thorough examination of the relative effectiveness of orthodontic adhesives and sealants in orthodontic treatment by following accepted criteria and methods.
Six studies assessing the effectiveness of various adhesive types in orthodontic bracket bonding are summarized in [Table 1]. In a clinical trial using 542 brackets,[22] O'brien et al. discovered similar failure rates of 4.7% for adhesives that were light-cured and 6.0% for those that were chemically cured. Glass ionomer cement (GIC) has a higher failure rate (36%) than diacrylate (15%), even though GIC requires less cleanup time. This was noted by Norevall et al.[23] compared to Fuji Ortho LC,[24] found that Light Bond adhesive formed stronger bonds and had comparable failure rates after 1.3 years. According to Shalini et al.[25] decalcification was less in compomer-bonded brackets but failure rates were similar (17% for compomer and 20% for resin adhesive). In comparison to glass ionomer cement,[11] observed that composite resin had a higher shear bond strength, particularly when reinforced. There is no discernible difference in bracket failure rates between primer-less and primer-based adhesives, according to.[26] These studies, which show differences in failure rates, cleanup durations, and bonding strengths among different adhesive types, emphasize the significance of considering both bonding efficacy and clinical results when choosing orthodontic adhesives.
Results
After identifying 1465 relevant article from various databases, only 6 articles that met the inclusion criteria of the present systematic review were included in the study ([Table 1]). A description of the adhesive types utilized in different experiments is given in [Table 2], along with a breakdown of each adhesive's performance analysis and the proportion of brackets bonded using it. It draws attention to the variety of adhesive materials used in orthodontics and the corresponding failure rates of each. For example, the failure rates of light-cured materials and traditional resin adhesives are similar, but the failure rate of glass ionomer cement (GIC) is significantly greater. Furthermore, research indicates that specific adhesive varieties, like compomer and composite resin, can provide benefits over more conventional choices like GIC, such as less decalcification and increased shear bond strength.
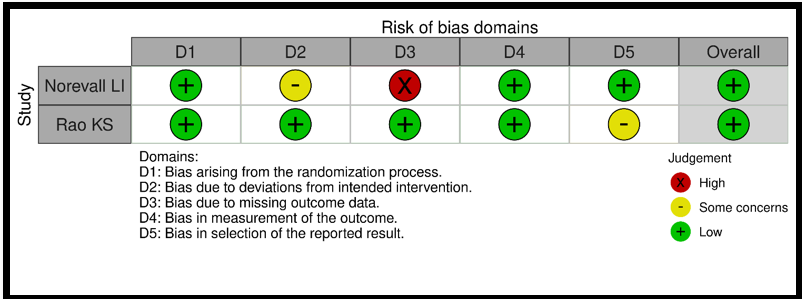
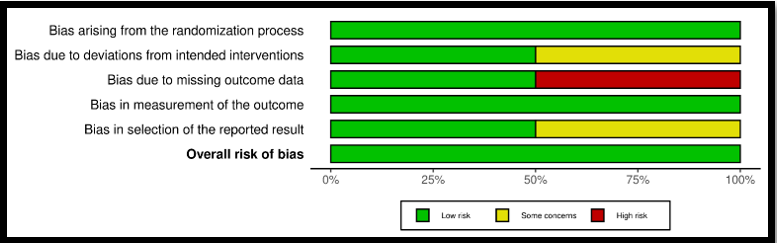
Risk of bias assessment was done for clinical study using the Cochrane's RoB2 tool and studies were found to be of low-risk bias and the methodology was found to be of good quality as is evident from [Figure 2], [Figure 3]. shows risk of bias assessment based on the RoB2 tool. This revealed that there was a higher risk in the missing data category and the moderate risk was observed under the deviation from the intended outcome and bias in the selection of the intended results.
Discussion
Bonding orthodontic brackets is an essential part of orthodontic treatment, depending greatly on the effectiveness and dependability of adhesives for successful results and patient contentment. When choosing adhesive for patients, clinicians need to weigh factors like bonding strength, failure rates, cleanup ease, and enamel protection among the many options available. This systematic review seeks to offer a thorough examination and comparison of the efficacy of various orthodontic adhesives as per recent research.
Bonding strength and failure rates
It is essential to select the correct orthodontic adhesive to achieve a good success rate of the treatment incurred to the patient. Since bonding strength and failure rates are important aspects that needs to be considered during a treatment procedure, a good orthodontic adhesive is imperative for the procedure.[22] had conducted a clinical study to compare light-cured and chemically-cured adhesives. They found that both had comparable failure rates that ranged from 4.7% to 6.0% respectively. This implies that both types of adhesives are effective in bonding brackets, showcasing their practicality in clinical settings. In a similar manner,[26] discovered similar rates of bracket failure with both a new primer-less adhesive and an old primer-based adhesive, reinforcing the dependability of current adhesive technologies.[23] found that glass ionomer cement (GIC) had a failure rate of 36%, which was significantly higher than diacrylate at 15%. Even though GIC has the benefit of needing shorter cleanup time, its lower bond strength raises doubts about its dependability in real-world situations. On the other hand,[24] found similar rates of failure between Fuji Ortho LC and Light Bond after 1.3 years in clinical trials, indicating comparable performance despite variations in shear bond strengths seen in laboratory tests.[25] conducted a comparison of the shear bond strength of orthodontic brackets using various adhesives and observed differences in bonding effectiveness between the adhesives examined. This highlights the significance of considering both failure rates and bonding strength when choosing orthodontic adhesives for bracket bonding. After conducting research,[27] found no appreciable differences in bond strength or failure rates between the experimental and conventional resins utilized to bond orthodontic brackets. During a 24-month period, the bonding efficiency and survival rates of both adhesives shown similar performance. As a result, orthodontic patients can successfully use both adhesives to bind brackets.[28] used finite element simulations and in vitro mechanical testing to compare the shear bond strengths of two orthodontic resins. The resins' bond strengths were comparable, according to the results, with Enlight® showing a higher strength because of its better mechanical retention. The adhesive layer's stress distribution was discovered by finite element analysis, and this information pointed to the resin-bracket interface as the most likely location for adhesive failure. The study emphasizes how crucial it is to consider both resin characteristics and bracket design to achieve the best bonding efficacy possible in orthodontics.
Recent research has provided important information on the effectiveness of adhesive used in orthodontics.[1] assessed adhesive resin for attaching orthodontic brackets, with positive findings regarding bonding effectiveness and clinical results. This emphasizes how adhesive materials in orthodontics are still developing and influencing treatment results. In addition,[29] carried out a systematic review and meta-analysis to compare the rates of clinical bracket failure using various bonding techniques. The results they discovered gave a detailed understanding of the effectiveness of different bonding techniques, helping healthcare providers choose the right adhesive with knowledge.In their study[30] explored the bonding resilience and remineralization effectiveness of a titanium tetrafluoride-containing orthodontic adhesive, underscoring the significance of adhesive makeup in boosting bonding capability and supporting enamel well-being in orthodontic care. Thus, recent studies have increased our knowledge of orthodontic adhesives, emphasizing their various features and practical implications. When choosing the right adhesive for a patient, clinicians should consider bonding strength, failure rates, and adhesive composition to improve treatment results and ensure patient satisfaction.
Enamel protection and decalcification
It is crucial to prioritize maintaining enamel health during orthodontic treatment in to avoid demineralization and decay. Research that compares various types of adhesive materials reveals their effects on enamel conservation and the effectiveness of treatment. In their study,[31] found that compomer and resin adhesive had comparable failure rates, but compomer may result in decreased decalcification. This implies that compomer might have benefits in maintaining enamel health while undergoing orthodontic treatment in comparison to resin adhesive. Likewise,[32] found that composite resin had higher shear bond strength compared to both types of glass ionomer cement, indicating its ability to create strong bonds while also preserving enamel surfaces.[31] examined a compomer and a resin-modified glass ionomer cement for orthodontic bonding, reinforcing the need to prioritize enamel protection when choosing adhesives. [33] carried out research to compare the adhesive bond strength of orthodontic brackets on newly extracted adult bovine teeth using various adhesives. Differences in bond strength were observed among the adhesives tested, with certain ones showing better adhesion to enamel than others. This emphasizes the importance of carefully evaluating and choosing adhesives that can offer sufficient bonding strength and safeguard enamel. The research conducted by Ireland and Sherriff.[1] Assessed the effectiveness of an adhesive resin in attaching orthodontic brackets and discovered positive outcomes regarding bonding efficiency and performance in clinical settings. This highlights the significance of considering the distinct properties and qualities of various adhesive materials to achieve the best orthodontic results. When clinicians choose the appropriate adhesive for their patients, they need to consider factors such as bonding strength, failure rates, and enamel protection. Furthermore, continuous research and structured assessments are needed to offer thorough understanding of the effectiveness of orthodontic adhesives and their significance in orthodontic treatment.[8] Condò et al. Performed a thorough examination and statistical analysis to assess how effective sealants and bonding materials are in preventing enamel demineralization in fixed orthodontic treatment. Their results offer important information for medical professionals when choosing materials that not just guarantee successful bonding but also protect enamel health during treatment.[34] studied the physical and chemical processes related to the adhesion of orthodontic bonding composites, providing clinicians with more insight into the factors affecting adhesive effectiveness and enamel safeguarding. Thus, maintaining enamel health is crucial in orthodontic care, and choosing the right adhesive materials is essential for success in this objective. By considering the results of different studies and continual research, healthcare providers can make educated choices to enhance treatment results and guarantee patient contentment.
Conclusion
Comparing orthodontic adhesives for bracket bonding reliability reveals important insights into enamel preservation and treatment effectiveness in orthodontic care. The potential benefits of compomer and composite resin adhesive materials in orthodontic treatment include reducing enamel decalcification while maintaining strong bonding strength for patients. However, it is crucial to recognize the constraints of current research, such as differences in approaches, participant numbers, and medical environments, that could impact the applicability of the results. Thus, the knowledge of how different adhesive materials perform over long periods is restricted due to the absence of long-term follow-up data. Future studies should concentrate on overcoming these restrictions by carrying out extensive clinical trials with standardized methods and prolonged follow-up evaluations. Moreover, delving deeper into the underlying mechanisms of enamel protection and adhesive bonding strength will advance our understanding and aid in the creation of better orthodontic adhesive materials. From a clinical perspective, the results of this research are important for orthodontists when choosing the appropriate adhesive materials that align with the specific needs and treatment objectives of their patients. Clinicians can enhance treatment results and reduce the risk of enamel demineralization during orthodontic treatment by evaluating factors like bonding strength, failure rates, cleanup convenience, and enamel protection. Continued research is needed to enhance our knowledge and create new solutions for better enamel protection and treatment effectiveness in orthodontics, despite improvements in adhesive materials.
Source of Funding
None.
Conflict of Interest
None.
References
- Ireland A, Sherriff M. Use of an adhesive resin for bonding orthodontic brackets. Eur J Onhod. 1994;16(1):27-34. [Google Scholar]
- Leizer C, Weinstein M, Borislow A, Braitman L. Efficacy of a filled-resin sealant in preventing decalcification during orthodontic treatment. Am J Orthod Dentofac Orthop. 2010;137(6):796-800. [Google Scholar]
- Gange P. The evolution of bonding in orthodontics. Am J Orthod Dentofa Orthop. 2015;147(4):56-63. [Google Scholar]
- Kravitz N, Dalloul B, Zaid Y, Shah C, Vaid N. What percentage of patients switch from Invisalign to braces? A retrospective study evaluating the conversion rate, number of refinement scans, and length of treatment. Am J Orthod Dentofac Orthop. 2023;163(4):526-30. [Google Scholar]
- Vaid N, Doshi V, Vandekar M. What’s “Trend”ing in Orthodontic literature? APOS Trends in Orthodontics. Asian Pacific Orthod Soc. 2016;6(1):1-4. [Google Scholar]
- Adel S, Vaid N, El-Harouni N, Kassem H, Zaher A. TIP, Torque & Rotations : How accurately do digital superimposition software packages quantify tooth movement?. Prog Orthod. 2022;23(1). [Google Scholar]
- Vaid N. Artificial Intelligence (AI) driven orthodontic care: A quest toward utopia?. Semin Orthod. 2021;27(2):57-61. [Google Scholar]
- Kamber R, Lueckel H, Kloukos D, Tennert C, Wierichs R. Efficacy of sealants and bonding materials during fixed orthodontic treatment to prevent enamel demineralization: a systematic review and meta-analysis. . Sci Rep. 2021;11(1). [Google Scholar]
- Minervini G, Marrapodi M, Cicciù M. Online Bruxism-related information: Can people understand what they read? A Cross-Sectional Study. J Oral Rehabil. 2023;50(11):1211-7. [Google Scholar]
- Alshadidi A, Aldosari L, Chaturvedi S, Saini R, Hassan S, Minervini G. Investigation on the application of artificial intelligence in prosthodontics.. Applied Sci. 2023;13 (8). [Google Scholar]
- Minervini G, Franco R, Marrapodi M, Fiorillo L, Cervino G, Cicciù M. The association between parent education level, oral health, and oral-related sleep disturbance. An observational crosssectional study. Eur J Paediatr Dent. 2023;24(3):218-41. [Google Scholar]
- Almeida L, Cicciù M, Doetzer A, Beck M. Mandibular condylar hyperplasia and its correlation with vascular endothelial growth factor. Journal of Oral Rehabil. 2023;50(9):845-51. [Google Scholar]
- AL, MA, UH, MP. Occurrence of Temporomandibular Disorders among patients undergoing treatment for Obstructive Sleep Apnoea Syndrome (OSAS) using Mandibular Advancement Device (MAD): A Systematic Review conducted according to PRISMA guidelines and the Cochrane handbook for systematic reviews of interventions.. J Oral Rehabil. 2023;50:1554-63. [Google Scholar]
- Rapone B, AI, Trasarti S, Ferrara E, Qorri E, Mancini A. Long-Term Outcomes of Implants Placed in Maxillary Sinus Floor Augmentation with Porous Fluorohydroxyapatite (Algipore® FRIOS®) in Comparison with Anorganic Bovine Bone (Bio-Oss®) and Platelet Rich Plasma (PRP): A Retrospective Study. J Clin Med. 2023;11(9). [Google Scholar]
- Kolstad JA, Cianciolo D, Ostertag A, Berzins D. Orthodontic Bond Strength Comparison between Two Filled Resin Sealants. Turk J Orthod. 2020;33(3):165-70. [Google Scholar]
- Bori E, Deslypere C, Muñoz E, Innocenti L. Clinical Results of the Use of Low-Cost TKA Prosthesis in Low Budget Countries-A Narrative Review. Prosthesis. 2023;5(3):840-50. [Google Scholar]
- Reddy N, Vempalli S, Prakash J, Suganna M, Meenakshi S, Shivakumar G. Evaluation of the Effect of Digital Dentistry on the Accuracy of Implant Placement and Prosthesis Fabrication-A Systematic Review and Meta-Analysis.. Prosthesis. 2023;5(3):666-77. [Google Scholar]
- Wellington I, Kaufman C, Antonacci C, Coskun E, Cote M, Singh H. The Effects of Interbody Device Design and Placement on Lumbar Lordosis and Disc Height in Transforaminal Lumbar Interbody Fusion. Prosthesis. 2023;5(3):752-62. [Google Scholar]
- Vozzo L, Azevedo L, Fernandes J, Fonseca P, Araújo F, Teixeira W. The Success and Complications of Complete-Arch Implant-Supported Fixed Monolithic Zirconia Restorations: A Systematic Review. Prosthesis. 2023;5(2):425-36. [Google Scholar]
- Pasta S. Silico Analysis of the Mitra Clip in a Realistic Human Left Heart Model. Prosthesis. 2023;5(3):876-87. [Google Scholar]
- Alkahtany M, Beatty M, Alsalleeh F, Petro T, Simetich B, Zhou Y. Color Stability, Physical Properties and Antifungal Effects of ZrO2 Additions to Experimental Maxillofacial Silicones: Comparisons with TiO2. Prosthesis . 2023;5(3):916-38. [Google Scholar]
- O’brien K, Orth D, Read M, Sandison R, Roberts C. A visible light-activated direct-bonding material: An in vivo comparative study. Am J Orthod Dentofac Orthop. 1989;95(4):348-51. [Google Scholar]
- Norevall L, Marcusson A, Persson M. A clinical evaluation of a glass ionomer cement as an orthodontic bonding adhesive compared with an acrylic resin. Eur J Orthod. 1996;18(4):373-84. [Google Scholar]
- Summers A, Kao E, Gilmore J, Gunel E, Ngan P. Comparison of bond strength between a conventional resin adhesive and a resin-modified glass ionomer adhesive: An in vitro and in vivo study. Am J Orthod Dentofac Orthop. 2004;126(2):200-6. [Google Scholar]
- Shalini S, Jha A, Kashyap P, Gupta P, Rajbhoj S, Bhandari S. A Comparison of the Shear Bond Strength of Orthodontic Brackets Bonded With Different Orthodontic Adhesives.. Cureus. 2023;3(2):29-33. [Google Scholar]
- Ramsundar K, Jain R, Balakrishnan N, Vikramsimha B. Comparative evaluation of bracket bond failure rates of a novel non-primer adhesive with a conventional primer-based orthodontic adhesive - a pilot study. J Dent Res Dent Clin Dent Prosp. 2023;17(1):35-44. [Google Scholar]
- Naqvi Z, Shaikh S, Pasha Z. Evaluation of Bond Failure Rate of Orthodontic Brackets Bonded with Green Gloo-Two Way Color Changes Adhesive: A Clinical Study. Ethiop J Health Sci. 2019;29(2):187-94. [Google Scholar]
- Avila A, Hecke M, Franco ADO, Vasco M, Oliveira D, Tanaka O. Comparative analysis of adhesive failure of orthodontic resins: An in vitro mechanical test with the finite element method. Eur J Gen Dent. 2013;2(2):124-33. [Google Scholar]
- Dudás C, Czumbel L, Kiss S, Gede N, Hegyi P, Mártha K. Clinical bracket failure rates between different bonding techniques: A systematic review and meta-Analysis. Eur J Orthod. 2023;45(2):175-85. [Google Scholar]
- Khalifa O, Badawi M, Soliman T. Bonding durability and remineralizing efficiency of orthodontic adhesive containing titanium tetrafluoride: an invitro study. BMC Oral Health. 2023;23(1). [Google Scholar]
- Millett D, Cluskey LM, McAuley F, Creanor S, Newell J, Love J. A comparative clinical trial of a compomer and a resin adhesive for orthodontic bonding. Resin Adh Orthod Bonding. 2000;70(3):233-40. [Google Scholar]
- Rao K, Reddy P, Yugandhar T, Reddy C, Kumar S. Comparison of shear bond strength of resin reinforced chemical cure glass ionomer, conventional chemical cure glass ionomer and chemical cure composite resin in direct bonding systems: An in vitro study. J Contemp Dent Pract. 2013;14(1):21-6. [Google Scholar]
- Czyzewsk A, Szanie Z, Olszewska A, Polichnowska M, Grabarek B, Dudek D. Comparison of Bond Strength of Orthodontic Brackets onto the Tooth Enamel of 120 Freshly Extracted Adult Bovine Medial Lower Incisors Using 4 Adhesives: A Resin-Modified Glass Ionomer Adhesive, a Composite Adhesive, a Liquid Composite Adhesive, and a One-Step Light-Cured Adhesive. Medical Sci Monitor. 2022;28. [Google Scholar]
- Condò R, Mampieri G, Cioffi A, Cataldi M, Frustaci I, Giancotti A. Physical and chemical mechanisms involved in adhesion of orthodontic bonding composites: in vitro evaluations. BMC Oral Health. 2021;21(1). [Google Scholar]
- Abstract
- Introduction
- Evaluation of orthodontic adhesives
- Challenges in enamel protection
- Clinical considerations, current landscape
- Materials and Methods
- Research question
- Search strategy
- Inclusion criteria
- Exclusion criteria
- Data extraction, synthesis, and quality assessment
- Risk of bias assessment
- Results
- Discussion
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Subramanian AK, Marrapodi MM, Ronsivalle V, Uzunçıbuk H, Russo D, Cicciù M, Minervini G. Comparative analysis of orthodontic adhesives for bracket bonding reliability: A systematic review [Internet]. J Contemp Orthod. 2025 [cited 2025 Sep 16];9(1):7-20. Available from: https://doi.org/10.18231/j.jco.2025.003
APA
Subramanian, A. K., Marrapodi, M. M., Ronsivalle, V., Uzunçıbuk, H., Russo, D., Cicciù, M., Minervini, G. (2025). Comparative analysis of orthodontic adhesives for bracket bonding reliability: A systematic review. J Contemp Orthod, 9(1), 7-20. https://doi.org/10.18231/j.jco.2025.003
MLA
Subramanian, Aravind Kumar, Marrapodi, Maria Maddalena, Ronsivalle, Vincenzo, Uzunçıbuk, Hande, Russo, Diana, Cicciù, Marco, Minervini, Giuseppe. "Comparative analysis of orthodontic adhesives for bracket bonding reliability: A systematic review." J Contemp Orthod, vol. 9, no. 1, 2025, pp. 7-20. https://doi.org/10.18231/j.jco.2025.003
Chicago
Subramanian, A. K., Marrapodi, M. M., Ronsivalle, V., Uzunçıbuk, H., Russo, D., Cicciù, M., Minervini, G.. "Comparative analysis of orthodontic adhesives for bracket bonding reliability: A systematic review." J Contemp Orthod 9, no. 1 (2025): 7-20. https://doi.org/10.18231/j.jco.2025.003
