- Visibility 52 Views
- Downloads 12 Downloads
- DOI 10.18231/j.jco.2025.010
-
CrossMark
- Citation
Assessment of mandibular buccal shelf and infrazygomatic crest bone thicknesses and densities in patients with different vertical facial heights- A CBCT study
Introduction
Temporary Anchorage Devices (TADs) for skeletal anchorage have been widely used with excellent effectiveness in recent years. Complex tooth movements have become easier and more predictable with the application of TADs. According to Choi and Park et al. TADs are a cost-effective solution that offers a secure and dependable method for attaining the intended tooth repositioning.[1] The TAD anchorage system gained widespread popularity due to the efforts of Kanomi et al. and Melsen et al. since 1998, used the concept of gaining anchorage from infra zygomatic crest for intrusion and retraction.[2], [3] However, the infra zygomatic crest screws were developed by Dr. Eric Liou from Taiwan in recent years, adding hope to overcome the limitations of existing TADs.[4]
Extra-alveolar sites, located further away from dental roots, tend to have higher bone density.[1] This results in increased primary stability of TAD.[1] The Mandibular Buccal Shelf (MBS) and the Infrazygomatic Crest (IZC) are two of the most frequently utilized extra-alveolar regions.[5]
The infrazygomatic crest consists of two cortical plates-buccal cortical plate and the floor of the lateral wall of the maxillary sinus. According to Baumgaertal S, Hans MG, placing miniscrews in this region could penetrate the maxillary sinus.[6] According to Reiser et al., when the miniscrew extends less than 2mm into the maxillary sinus, the Schneiderian sinus membrane becomes elevated, favours blood clot formation and aids in healing. When the miniscrew extends more than 2mm into the sinus, it perforates the membrane and disrupts healing, increasing the incidence of sinusitis.[7]
Previous studies show that variation in vertical facial dimension of the patients’ has an impact on the maxillary sinus and the alveolar bone width.[8], [9] Thus, it can be helpful to consider the impact of vertical facial dimension when using extra-alveolar miniscrews for patients with varying vertical profiles.
Multiple factors associated with the failure of miniimplants have been previously investigated. These factors include the placement site, the operator's experience, oral hygiene, bone thickness, and bone density.[10] In a study conducted by Chang and Tseng (2014), it was found that there is a strong relationship between bone density and the potential for anchorage at the site.[11] Additionally, the stability of miniimplants in sites with insufficient cortical bone thickness seems to be affected by the cortical anchorage provided by bone density.[12]
Therefore, this investigation aims to assess the thickness and density of the bone in the Mandibular Buccal Shelf (MBS) and the Infrazygomatic Crest (IZC) through the utilization of Cone-Beam Computed Tomography (CBCT). This analysis will be conducted on individuals with diverse vertical facial heights, with the ultimate goal of determining the most suitable location for the placement of temporary anchorage devices (TAD).
|
|
Groups |
No. of samples |
Mean ± SD |
P-Value |
|
IZC |
Group 1 |
10 |
754 ± 45.9 |
0.01 |
|
Group 2 |
10 |
861.1 ± 77.8 |
||
|
Group 3 |
10 |
1149.7 ± 49.4 |
||
|
MBS 1st molar |
Group 1 |
10 |
811.3 ± 15.4 |
0.01 |
|
Group 2 |
10 |
1192.4 ± 38.3 |
||
|
Group 3 |
10 |
1480.2 ± 48.6 |
||
|
MBS 2nd molar |
Group 1 |
10 |
887.5 ± 46.2 |
0.01 |
|
Group 2 |
10 |
1207.4 ± 41.4 |
||
|
Group 3 |
10 |
1543.4 ± 45.4 |
|
Group |
1st Molar(Mean ± SD) |
2nd Molar(Mean ± SD) |
P-Value |
|
Group 1 |
811.3 ± 15.4 |
887.5 ± 46.2 |
0.001 |
|
Group 2 |
1192.4 ± 38.3 |
1207.4 ± 41.4 |
0.41 |
|
Group 3 |
1480.2 ± 48.6 |
1543.4 ± 45.4 |
0.0076 |
|
Groups |
Sites |
No.of samples |
Mean |
SD |
P-Value |
|
Group 1 |
MB70 |
10 |
2.17 |
0.17 |
< 0.001 |
|
MB65 |
10 |
1.60 |
0.31 |
||
|
DB70 |
10 |
2.11 |
0.16 |
||
|
DB65 |
10 |
1.77 |
0.19 |
||
|
PR70 |
10 |
3.91 |
0.56 |
||
|
PR65 |
10 |
2.93 |
0.28 |
||
|
Group 2 |
MB70 |
10 |
3.18 |
0.21 |
< 0.001 |
|
MB65 |
10 |
2.44 |
0.27 |
||
|
DB70 |
10 |
3.49 |
0.31 |
||
|
DB65 |
10 |
2.84 |
0.20 |
||
|
PR70 |
10 |
5.38 |
0.29 |
||
|
PR65 |
10 |
4.40 |
0.21 |
||
|
Group 3 |
MB70 |
10 |
3.54 |
0.21 |
< 0.001 |
|
MB65 |
10 |
2.82 |
0.19 |
||
|
DB70 |
10 |
3.65 |
0.24 |
||
|
DB65 |
10 |
3.08 |
0.13 |
||
|
PR70 |
10 |
5.65 |
0.31 |
||
|
PR65 |
10 |
4.72 |
0.30 |
||
|
Maxilla |
Group 1Mean ± SD |
Group 2Mean ± SD |
Group 3Mean ± SD |
P-Value |
|
MB70 |
2.2 ± 0.2 |
3.2 ± 0.2 |
3.5 ± 0.2 |
< 0.01 |
|
MB65 |
1.6 ± 0.3 |
2.4 ± 0.3 |
2.8 ± 0.2 |
< 0.01 |
|
DB70 |
2.1 ± 0.2 |
3.5 ± 0.3 |
3.7 ± 0.2 |
< 0.01 |
|
DB65 |
1.8 ± 0.2 |
2.8 ± 0.2 |
3.1 ± 0.1 |
< 0.01 |
|
PR70 |
3.9 ± 0.6 |
5.4 ± 0.3 |
5.7 ± 0.3 |
< 0.01 |
|
PR65 |
2.9 ± 0.3 |
4.4 ± 0.2 |
4.7 ± 0.3 |
< 0.01 |
|
Sites |
Group 1 Mean ± SD |
Group 2 Mean ± SD |
Group 3 Mean ± SD |
P-Value |
|
2MDH6 |
1.1 ± 0.1 |
2.6 ± 0.4 |
3.8 ± 0.6 |
P (<0.01) |
|
2MDH11 |
4.1 ± 0.6 |
4.3 ± 0.4 |
5.7 ± 0.6 |
P (<0.01) |
|
2MMH6 |
1.6 ± 0.4 |
2 ± 0.4 |
3 ± 0.4 |
P (<0.01) |
|
2MMH11 |
2.3 ± 0.4 |
2.7 ± 0.3 |
4.1 ± 0.5 |
P (<0.01) |
|
2MDV4 |
9.7 ± 0.8 |
10.7 ± 0.6 |
12 ± 0.6 |
P (<0.01) |
|
2MDV5 |
11.6 ± 0.9 |
12.8 ± 0.7 |
14.1 ± 0.5 |
P (<0.01) |
|
2MMV4 |
11 ± 0.5 |
11.8 ± 0.4 |
12.9 ± 0.4 |
P (<0.01) |
|
2MMV5 |
8.8 ± 0.6 |
9.2 ± 0.4 |
10.4 ± 0.5 |
P (<0.01) |
|
1MDH6 |
1.6 ± 0.4 |
1.9 ± 0.3 |
1.6 ± 0.4 |
P (<0.01) |
|
1MDH11 |
2.3 ± 0.4 |
2.8 ± 0.3 |
2.3 ± 0.4 |
P (<0.01) |
|
1MMH6 |
1.4 ± 0.2 |
1.8 ± 0.2 |
2.4 ± 0.2 |
P (<0.01) |
|
1MMH11 |
1.9 ± 0.4 |
2.1 ± 0.2 |
2.7 ± 0.2 |
P (<0.01) |
|
1MDV4 |
5.5 ± 0.6 |
6.9 ± 0.4 |
7.4 ± 0.4 |
P (<0.01) |
|
1MDV5 |
6.4 ± 0.5 |
7 ± 0.4 |
7.6 ± 0.4 |
P (<0.01) |
|
1MMV4 |
5.1 ± 0.6 |
6.5 ± 0.4 |
7 ± 0.4 |
P (<0.01) |
|
1MMV5 |
5 ± 0.5 |
6.2 ± 0.2 |
6.5 ± 0.4 |
P (<0.01) |
Materials and Methods
This was a retrospective, descriptive, observational study in which the infrazygomatic crest was evaluated in the vertical directions, and the mandibular buccal shelf was evaluated in both transverse and vertical directions through CBCT scans. For this study, CBCT scans were selected from patients aged at least 16 years whose skeletal growth had ceased and who had undergone CBCT imaging for orthodontic diagnosis and treatment. The sample size consisted of 90 patients.
The determination of the sample size was executed through the utilization of G Power statistical software. The G*Power software is commonly employed to compute sample size and power for a myriad of statistical techniques, including F, t, χ2, Z, and exact tests. Key assumptions for sample size were- Power -0.8 and 95% significance level.
The sample was characterized into three different groups based on their vertical facial pattern, which was analyzed by lateral cephalometric analysis based on the following parameters: Jaraback ratio, FMA [Tweed analysis], Y-axis (S-Gn: FH) [Down's analysis], Mandibular plane angle [Steiner’s analysis]. The skeletal maturity was assessed by the cervical vertebral maturation method. [13]
Group 1: Vertical growth pattern
Group 2: Average growth pattern
Group 3: Horizontal growth pattern
Patients with skeletal growth remaining, gross facial asymmetry, periodontal disease, maxillofacial trauma, syndromic individuals, medically compromised patients and patients who had undergone orthognathic surgery were excluded from the study.
The CBCT scans were obtained on campus using the I-CAT17-19 scanner in the Department of Oral Medicine and Radiology, Buddha Institute of Dental Sciences and Hospital, Patna.
The CBCT scanner was adjusted to the following specifications: A field view of at least 16cmx13cm, 120kV, 37.7 mAs, Voxel size of 0.25mm, and Exposure time of 13.68s. The tomographic exams were adjusted and analysed using Vision software (Image Science International). The images were analysed in axial, sagittal and coronal views.
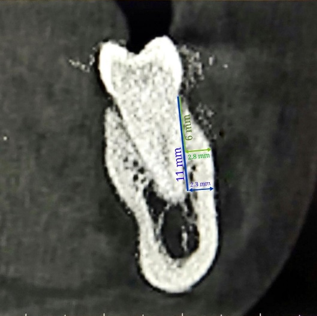
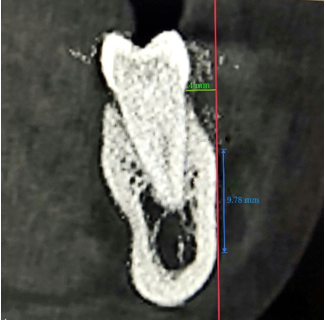
For the measurement of the buccal shelf and Infrazygomatic crest, the methods suggested by Vargas et al. were used.[14] The four roots of the mandibular first and second molars were assessed in the mandibular buccal shelf area. All roots were evaluated transversely and vertically. The standard miniscrew length is at least 6mm, and extra alveolar miniscrews are usually longer than 10mm; therefore, the transverse buccal bone thickness was evaluated apically at 6mm and 11mm from the cementoenamel junction (CEJ).[3], [15] [Figure 1] . The buccal bone thickness was evaluated at 4mm and 5mm from the CEJ. [Figure 2]
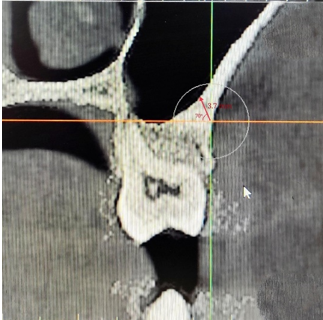
As suggested by Vargas et al., the maxillary left first molar's buccal root and the area between the first and second left molars, apical to the inter-radicular space, were assessed in the infrazygomatic crest region. [14] [Figure 3]. A previous research done by Dr Liou et al. suggested maximum bone thickness at 65o and 70o in the coronal view; therefore, the assessment at these two angles was selected for this study. [4]
The bone density was measured in Hounsefield scale (HU) in the infrazygomatic crest and mandibular buccal shelf in the 1st and 2nd molar region.
Statistical analysis
This procedure was duly authenticated, with an evaluation of intraobserver and interobserver errors carried out through a pilot study consisting of 5 tomographic exams where the IZC was analyzed. The measurements were all subjected to a reevaluation after 14 days. The intraclass correlation coefficient registered an average of 99.75%, with the interclass correlation coefficient recording 98%.
Descriptive Statistics: Data collected from this study was analyzed statistically as follows: i) Categorical variables presented in the form of frequency table along with percentage and graphical presentation wherever necessary. ii) Descriptive statistics were applied to quantitative variables, which included the mean, standard deviation and 95% confidence interval. Graphical representation was utilized as deemed appropriate. Inferential statistics: The normality of the data was statistically proven using the Kolmogorov-Smirnov test. ANOVA test was used to analyze the relation between the bone thickness of the mandibular buccal shelf and the infrazygomatic crest with different vertical facial heights. *No grants were taken for this study. It was self-funded. And there is no conflict of interest in this study.
Results
The current investigation was conducted in order to assess the thickness and density of the bone in the buccal shelf and infrazygomatic crest using Cone Beam Computed Tomography (CBCT) in subjects with varying vertical facial dimensions.
Bone density
As per the one-way ANOVA test, [Table 1] depicts a significant variation (P< 0.01) in density at IZC and MBS in the 3 different groups. The highest bone density (mean 1149.7 HU) at IZC was found in group 3, i.e. horizontal facial patterns. The bone density decreased significantly (P< 0.01) in group 2, i.e. average facial patterns, and was found to be the least in group 1, i.e. vertical facial patterns. Similarly, at MBS in the 1st molar region, the highest bone density (mean 1480.2 HU) was found in group 3, i.e. horizontal facial patterns. The bone density decreased significantly (P<0.01) in group 2, i.e. average facial patterns and was found to be the least in group 1, i.e. vertical facial patterns. MBS in the 2nd molar region had the highest bone density (mean 1543.4 HU) in group 3, i.e. horizontal facial patterns. The bone density decreased significantly (P< 0.01) in group 2, i.e. average facial patterns and was found to be the least in group 1, i.e. vertical facial patterns.
As per the two-way ANOVA test, [Table 2] depicts inter and intra-group comparisons of the density of MBS in the 1st and 2nd molar regions of 3 different groups. In Group 1, the difference in bone density between the 1st and 2nd molar regions was highly significant (P<0.001). In Group 2, the difference in bone density between 1st and 2nd molar regions was insignificant (P<0.41). In Group 3, the difference in bone density between 1st and 2nd molar regions was highly significant (P<0.0076).
Bone thickness-IZC
As per the one-way ANOVA test, [Table 3] depicts a significant variation (P< 0.001) between the mean values of bone thickness in different groups at different sites. In all the groups, maximum bone thickness was found at the interproximal site between 1st and 2nd molar at an insertion angle of 70o. In group 1, it was 3.91 mm (SD 0.56 mm), 2.38 mm (SD 0.29 mm) in group 2 and in group 3, it was 5.65 mm (SD 0.31 mm).
[Table 4] depicts a highly significant variation (P< 0.01) in bone thickness upon intergroup comparison between the 3 groups. Maximum bone thickness of 5.7 mm was found to be in group 3, i.e. horizontal growth pattern. In addition, it was found to be maximum at the interproximal area between 1st and 2nd molar.
Bone thickness- MBS
According to the descriptive statistics and intergroup comparison in [Table 5], the least transverse bone thickness (1.1 mm ± 0.1) was depicted in group 1 at the distal root of the 2nd molar at 6 mm from CEJ. The maximum transverse bone thickness (5.7 mm ± 0.6) was present in group 3 at the distal root of 2nd molar at 11mm from CEJ. The vertical bone thickness was significantly higher in group 3 at the distal root of the 2nd molar at 5 mm from CEJ. There was a significant (P <0.01) difference in vertical and transverse bone thickness among the 3 groups. The highest bone thickness was found in group 3 (horizontal facial pattern), and the least was found in group 1 (vertical facial pattern). The MBS bone thickness increased significantly (P <0.01) as we moved posteriorly from the mesial root of 1st molar towards the distal root of 2nd molar.
Discussion
The introduction of Temporary Anchorage Devices (TADs) has significantly enhanced the predictability of complex tooth movements. TADs provide secure anchorage and are cost-effective according to Choi-Park and Papadopoulos-Tarawneh. [16], [17] Factors like bone thickness and density affect TAD placement (Chun and Lim, 2009). This study aimed to identify optimal TAD sites based on bone density across different facial growth patterns.
Moon et al. and Sato et al. found higher bone density in molar regions of individuals with lower mandibular plane angles.[18] Miyawaki et al. reported similar results, especially in hypodivergent groups, emphasizing stability in specific areas like the infrazygomatic crest (IZC) and mandibular buccal shelf (MBS). [19]
Assessing TAD stability involves primary (insertion torque) and secondary (bone remodeling) stability. [20] Choi et al. highlighted insertion torque as crucial for TAD success. Quality of cortical bone, crucial for stability, should exceed 1.0 mm.[21] Previous studies by Chang et al. recommend specific TAD placements: MBS next to mandibular second molars for thicker bone and IZC buccal to maxillary molars for greater thickness. [22]
In conclusion, understanding bone density and thickness guides optimal TAD placement in MBS and IZC. Preliminary CBCT evaluation is crucial for successful TAD placement, considering both bone and soft tissue characteristics. CBCT imaging aids in planning TAD placement due to varying bone thickness in MBS and IZC with different facial patterns.
Conclusion
Bone density and thickness at MBS and IZC vary with vertical facial height. Horizontal growth patterns typically offer thicker and denser bone, influencing TAD suitability. CBCT-guided planning is crucial for safe and effective TAD placement
In this study, it was observed that the bone thickness and density at MBS and IZC were correlated with vertical facial heights. We can conclude our study with the following remarks:
Thickness and density of bone in the infrazygomatic crest and mandibular buccal shelf are related to varying vertical facial heights.
Patients with horizontal growth patterns had thicker and denser bone when compared to an average and vertical growth pattern in the infrazygomatic crest and mandibular buccal shelf area.
The MBS bone thickness increased significantly (P <0.01) as we moved posteriorly from the mesial root of 1st molar towards the distal root of 2nd molar. Higher bone density was found around 2nd permanent molar in the mandibular buccal shelf area.
More bone thickness was noticed in the horizontal growth pattern in comparison to the average and vertical growth pattern in the IZC region. At an angulation of 70o, more bone thickness was observed compared to 65o insertion angulation of TAD.
Source of Funding
None.
Conflict of Interest
None.
References
- JH Choi, CH Park, SW Yi, HJ Lim, HS Hwang. Bone density measurement in interdental areas with simulated placement of orthodontic miniscrew implants. Am J Orthod Dentofac Orthop 2009. [Google Scholar]
- R Kanomi. Mini-implant for orthodontic anchorage. J Clin Orthod 1997. [Google Scholar]
- B Melsen, A Costa. Immediate loading of implants used for orthodontic anchorage. Clin Orthod Res 2000. [Google Scholar]
- EJ Liou, PH Chen, YC Wang, JC Lin. A computed tomographic image study on the thickness of the infrazygomatic crest of the maxilla and its clinical implications for miniscrew insertion. . AmJ Orthod Dentofa Orthop 2007. [Google Scholar]
- CC Chang, JS Lin, HY Yeh. Extra-alveolar bone screws for conservative correction of severe malocclusion without extractions or orthognathic surgery. Curr Osteoporosis Rep 2018. [Google Scholar]
- S Baumgaertel, MG Hans. Buccal cortical bone thickness for mini-implant placement. Am J Orthod Dentofac Orthop 2009. [Google Scholar]
- GM Reiser, Z Rabinovitz, J Bruno, PD Damoulis, TJ Griffin. Evaluation of maxillary sinus membrane response following elevation with the crestal osteotome technique in human cadavers. Int J Oral Maxillofac Imp 2001. [Google Scholar]
- R Nucera, A Lo Giudice, AM Bellocchio, P Spinuzza, A Caprioglio, L Perillo. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. . Angle Orthod 2017. [Google Scholar]
- YK Lee, JW Kim, SH Baek, TW Kim, YI Chang. Root and bone response to the proximity of a mini-implant under orthodontic loading. Angle Orthod 2010. [Google Scholar]
- R Davo, C Malevez, J Rojas. Immediate function in the atrophic maxilla using zygoma implants: a preliminary study. . J Prosthe Dent 2007. [Google Scholar]
- C Chang, SS Liu, WE Roberts. Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva. . Angle Orthod 2015. [Google Scholar]
- T Elshebiny, JM Palomo, S Baumgaertel. Anatomic assessment of the mandibular buccal shelf for miniscrew insertion in white patients. Am J Orthod Dentofac Orthop 2018. [Google Scholar]
- JA Mcnamara, L Franchi. The cervical vertebral maturation method: A user's guide. . Angle Orthod 2018. [Google Scholar]
- EO Vargas, RL De Lima, LI Nojima. Mandibular buccal shelf and infrazygomatic crest thicknesses in patients with different vertical facial heights. Am J Orthod Dentofac Orthop 2020. [Google Scholar]
- B Wilmes, C Rademacher, G Olthoff, D Drescher. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop/Fortschritte der Kieferorthopädie 2006. [Google Scholar]
- SH Choi, CJ Hwang. Factors affecting the failure of TADs and efforts to improve the biomechanical stability of TADs. . Temporary anchorage devices in clinical orthodontics 2020. [Google Scholar]
- MA Papadopoulos, F Tarawneh. The use of miniscrew implants for temporary skeletal anchorage in orthodontics: a comprehensive review. . Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2007. [Google Scholar]
- CH Moon, DG Lee, HS Lee, JS Im, SH Baek. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. . Angle Orthod 2008. [Google Scholar]
- S Miyawaki, I Koyama, M Inoue, K Mishima, T Sugahara, T Takano-Yamamoto. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofac Orthop 2003. [Google Scholar]
- Y Chen, HM Kyung, WT Zhao, WJ Yu. Critical factors for the success of orthodontic miniimplants: a systematic review. Am J Orthod Dentofac Orthop 2009. [Google Scholar]
- SH Choi, CJ Hwang. Factors Affecting the Failure of TADs and Efforts to Improve the Biomechanical Stability of TADs. Temporary Anchorage Devices in Clinical Orthodontics 2020. [Google Scholar]
- CH Chang, JH Lin, WE Roberts. Success of infrazygomatic crest bone screws: patient age, insertion angle, sinus penetration, and terminal insertion torque. Am J Orthod Dentofac Orthop 2022. [Google Scholar]
